-
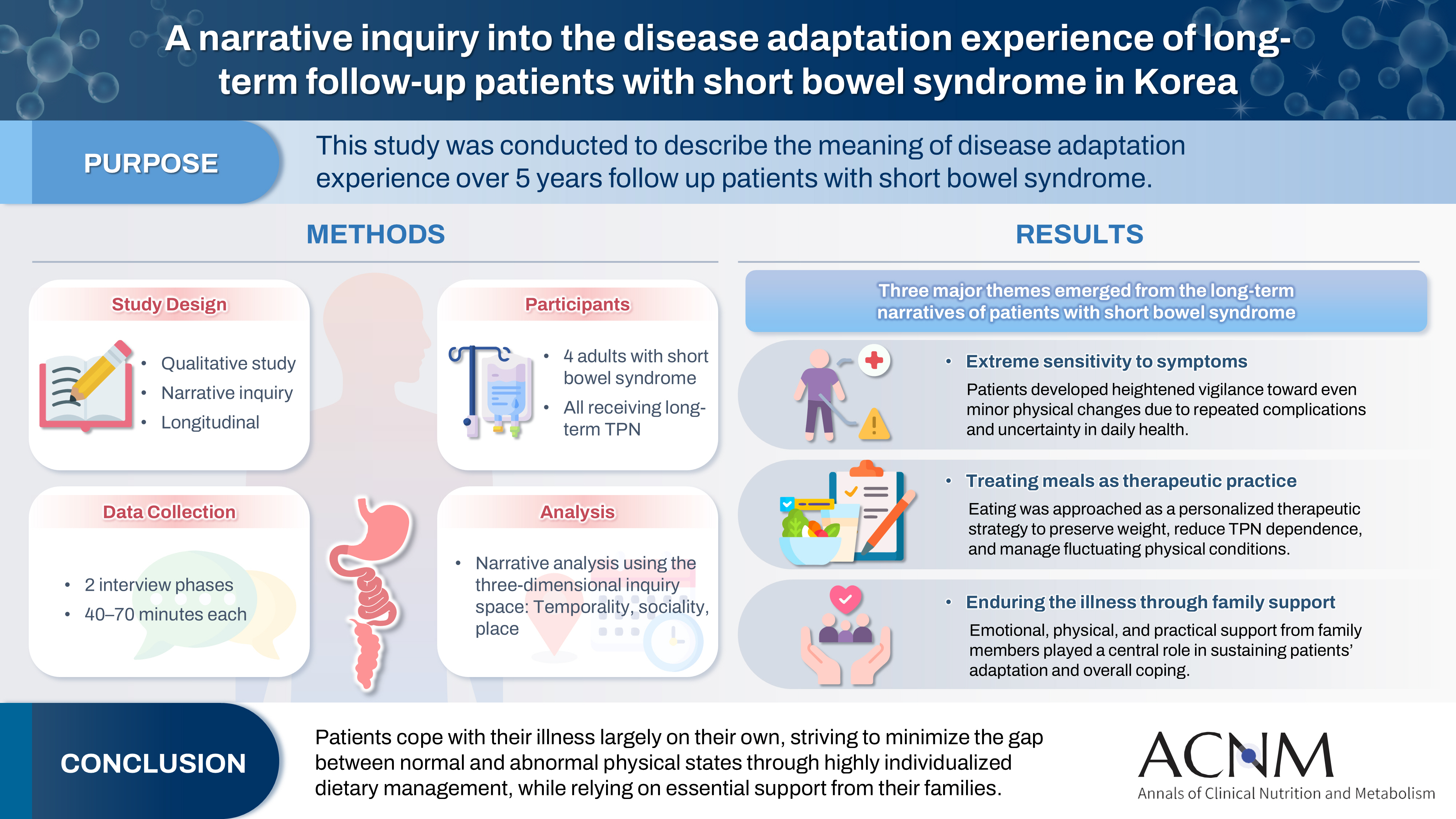
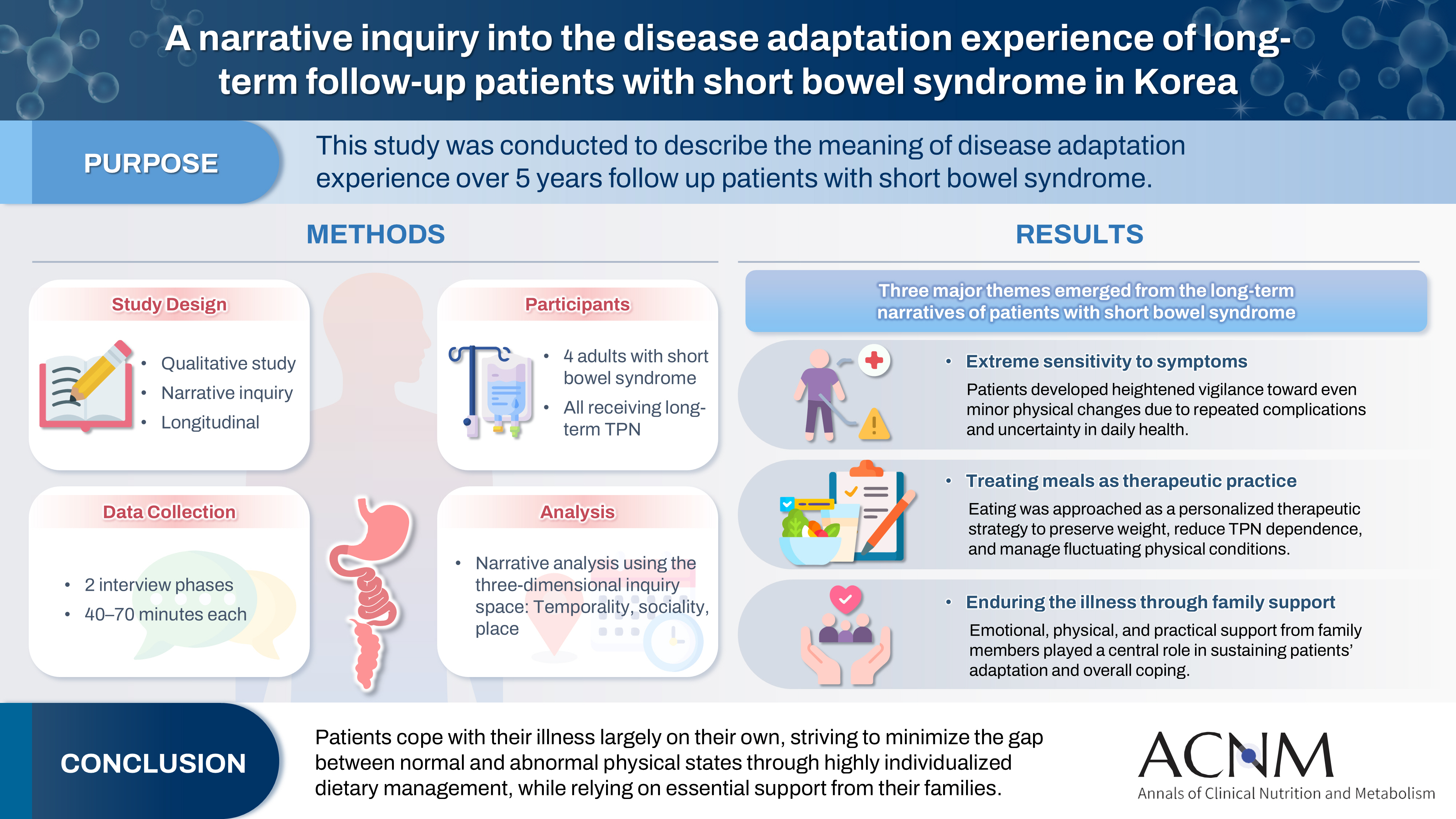
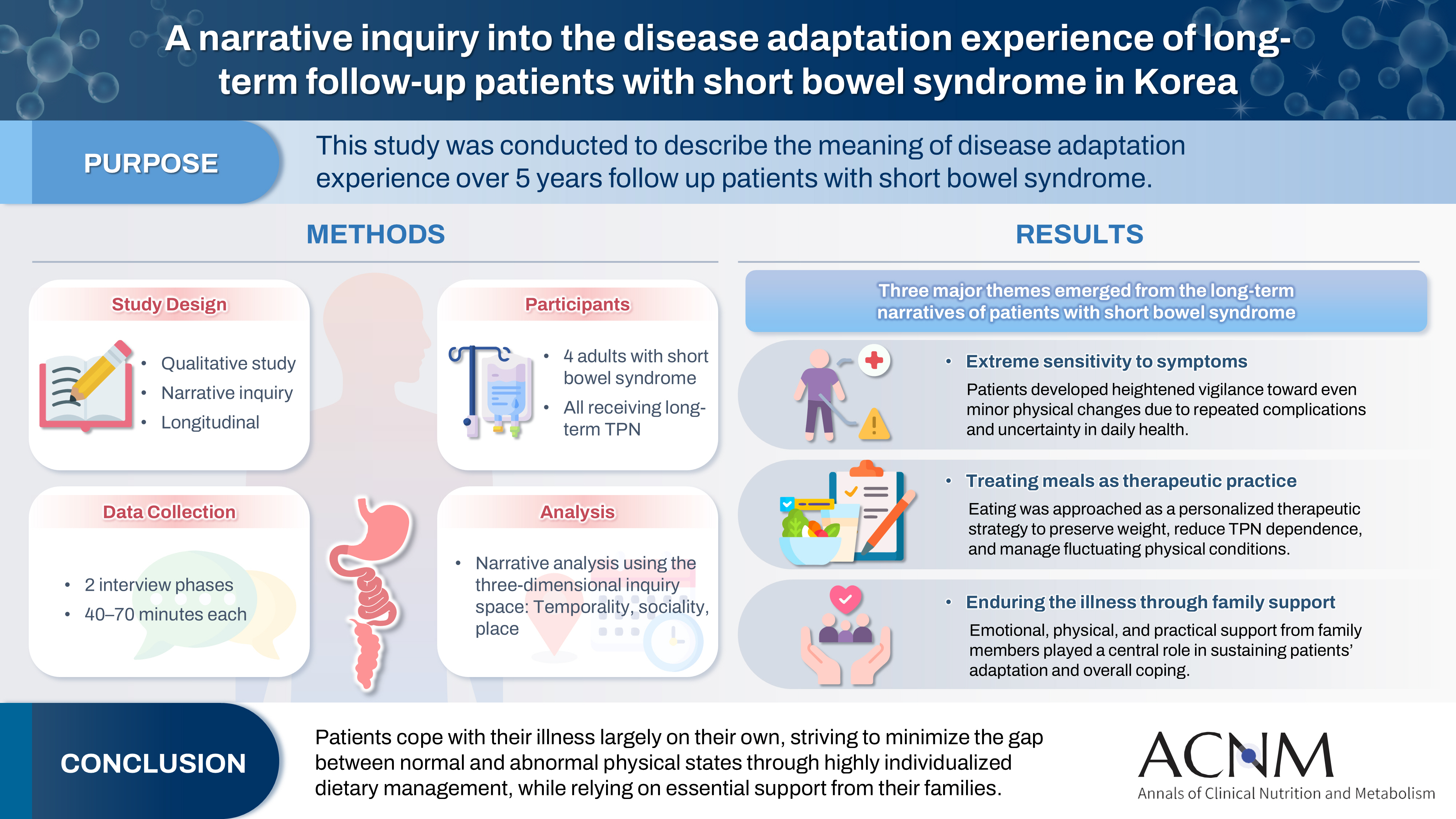
A narrative inquiry into the disease adaptation experience of long-term follow-up patients with short bowel syndrome in Korea
-
Eun-Mi Seol, Eunjung Kim
-
Ann Clin Nutr Metab 2025;17(3):188-195. Published online December 1, 2025
-
DOI: https://doi.org/10.15747/ACNM.25.0028
-
-
 Graphical Abstract Graphical Abstract
 Abstract Abstract
 PDF PDF Supplementary Material Supplementary Material
 - Purpose
This study was conducted to describe the meaning of disease adaptation experience over a 5-year long-term follow-up of patients with short bowel syndrome.
Methods
Four patients were recruited from a tertiary hospital in Korea. This study was conducted through first and second interviews from January 2019 to July 2022. The transcribed data were analyzed using narrative methods.
Results
The mean age of the participants was 64 years, and the mean treatment period after small bowel resection was 100 months. The participants lost a mean of 19.3 kg body weight and all were receiving home total parenteral nutrition 2–7 days a week. The meaning of the experience of adapting to the disease for patients was found to be “extremely sensitive to the symptoms,” “considering eating food as another effective treatment method,” and “enduring the disease through family affection.”
Conclusion
Patients are struggling alone to cope with physical symptoms and adapt to their disease. For this, they are doing their best to narrow the gap between normal and abnormal physical conditions by thoroughly implementing diet therapy according to their physical characteristics. This entire process is supported by their families.
-
A practical guide for enteral nutrition from the Korean Society for Parenteral and Enteral Nutrition: Part I. prescribing enteral nutrition orders
-
Ye Rim Chang, Bo-Eun Kim, In Seok Lee, Youn Soo Cho, Sung-Sik Han, Eunjung Kim, Hyunjung Kim, Jae Hak Kim, Jeong Wook Kim, Sung Shin Kim, Eunhee Kong, Ja Kyung Min, Chi-Min Park, Jeongyun Park, Seungwan Ryu, Kyung Won Seo, Jung Mi Song, Minji Seok, Eun-Mi Seol, Jinhee Yoon, Jeong Meen Seo, for KSPEN Enteral Nutrition Committee
-
Ann Clin Nutr Metab 2025;17(1):3-8. Published online April 1, 2025
-
DOI: https://doi.org/10.15747/ACNM.25.0002
-
-
 Abstract Abstract
 PDF PDF
- Purpose
This study aimed to develop a comprehensive practical guide for enteral nutrition (EN) designed to enhance patient safety and reduce complications in Korea. Under the leadership of the Korean Society for Parenteral and Enteral Nutrition (KSPEN), the initiative sought to standardize EN procedures, improve decision-making, and promote effective multidisciplinary communication.
Methods
The KSPEN EN committee identified key questions related to EN practices and organized them into seven sections such as prescribing, delivery route selection, formula preparation, administration, and quality management. Twenty-one experts, selected based on their expertise, conducted a thorough literature review to formulate evidence-based recommendations. Drafts underwent peer review both within and across disciplines, with final revisions completed by the KSPEN Guideline Committee. The guide, which will be published in three installments, addresses critical elements of EN therapy and safety protocols.
Results
The practical guide recommends that EN orders include detailed elements and advocates the use of electronic medical records for communication. Standardized prescription forms and supplementary safety measures are outlined. Review frequency is adjusted according to patient condition—daily for critically ill or unstable patients and as dictated by institutional protocols for stable patients. Evidence indicates that adherence to these protocols reduces mortality, complications, and prescription errors.
Conclusion
The KSPEN practical guide offers a robust framework for the safe delivery of EN tailored to Korea’s healthcare context. It emphasizes standardized protocols and interdisciplinary collaboration to improve nutritional outcomes, patient safety, and operational efficiency. Rigorous implementation and monitoring of adherence are critical for its success.
-
Citations
Citations to this article as recorded by  - Bridging evidence and clinical practice: a practical guide for enteral nutrition from the Korean Society for Parenteral and Enteral Nutrition
Suk-Kyung Hong
Ann Clin Nutr Metab.2025; 17(1): 1. CrossRef
-
5,941
View
-
175
Download
-
1
Crossref
-
Long-Term Changes of Body Mass Index and Nutritional Biochemical Markers in the Obese Elderly with Gastric Cancer
-
Eunjung Kim, Ji-Hyeon Park, Eun-Mi Seol, Seong-Ho Kong, Do Joong Park, Han-Kwang Yang, Hyuk-Joon Lee
-
Ann Clin Nutr Metab 2021;13(2):52-61. Published online December 31, 2021
-
DOI: https://doi.org/10.15747/ACNM.2021.13.2.52
-
-
 PDF PDF
-
In-line Filtration in Parenteral Nutrition
-
Eunjung Kim, Eun-Mi Seol
-
J Clin Nutr 2019;11(1):1-4. Published online June 30, 2019
-
DOI: https://doi.org/10.15747/jcn.2019.11.1.1
-
-
 Abstract Abstract
 PDF PDF
Metabolic abnormalities and catheter-related infections are common complications of parenteral nutrition (PN). Particulate contamination is a catheter-related complication can occur when administering PN: mixing the electrolytes, trace elements, vitamins into the PN, or puncturing a rubber stopper at the PN formulation. In addition, the aggregation of the components of the PN solution by a drug incompatibility reaction could be related to particulate contamination. PN contaminated with precipitates, insoluble particles, and bacteria was reported as the cause of the death of a patient. The Food and Drug Administration recommended that the filters be used during PN administration. In-line filters can retain the bacteria and insoluble particles in PN solutions, and prevent their infusion into the patient. Therefore, in-line filters are recommended to prevent catheter-related complications that can occur during PN infusion. A 0.2µ filter for lipid-free PN and a 1.2µ filter for lipid-containing PN solutions can be used. On the other hand, when a filter is applied, the infusion rate can decrease and the economic burden will increase for patients requiring long-term PN. In addition, small particles, such as viruses, polymers, and proteins cannot be filtered out completely. In conclusion, in-line filers are recommended to prevent catheter-related complications that can occur during PN administration, but there are no international standardized guidelines. Therefore, standardized guidelines will be needed based on evidence accompanied by clinical trials. In addition, in-line filter applications should be considered in the clinical field depending on the patient’s condition.
-
Nutritional Therapy Related Complications in Hospitalized Adult Patients: A Korean Multicenter Trial
-
Eun-Mi Seol, Kye Sook Kwon, Jeong Goo Kim, Jung-Tae Kim, Jihoon Kim, Sun-Mi Moon, Do Joong Park, Jung Hyun Park, Je Hoon Park, Ji Young Park, Jung-Min Bae, Seung Wan Ryu, Ji-Young Sul, Dong Woo Shin, Cheung Soo Shin, Byung Kyu Ahn, Soo Min Ahn, Hee Chul Yu, Gil Jae Lee, Sanghoon Lee, A Ran Lee, Jae Young Jang, Hyun Jeong Jeon, Sung Min Jung, Sung-Sik Han, Suk-Kyung Hong, Sun-Hwi Hwang, Yunhee Choi, Hyuk-Joon Lee
-
J Clin Nutr 2019;11(1):12-22. Published online June 30, 2019
-
DOI: https://doi.org/10.15747/jcn.2019.11.1.12
-
-
 Abstract Abstract
 PDF PDF
Purpose:Nutritional therapy (NT), such as enteral nutrition (EN) or parenteral nutrition (PN), is essential for the malnourished patients. Although the complications related to NT has been well described, multicenter data on symptoms in the patients with receiving NT during hospitalization are still lacking. Methods:Nutrition support team (NST) consultations, on which NT-related complications were described, were collected retrospectively for one year. The inclusion criteria were patients who were (1) older than 18 years, (2) hospitalized, and (3) receiving EN or PN at the time of NST consultation. The patients’ demographics (age, sex, body mass index [BMI]), type of NT and type of complication were collected. To compare the severity of each complication, the intensive care unit (ICU) admission, hospital stay, and type of discharge were also collected. Results:A total of 14,600 NT-related complications were collected from 13,418 cases from 27 hospitals in Korea. The mean age and BMI were 65.4 years and 21.8 kg/m2. The complications according to the type of NT, calorie deficiency (32.4%, n=1,229) and diarrhea (21.6%, n=820) were most common in EN. Similarly, calorie deficiency (56.8%, n=4,030) and GI problem except for diarrhea (8.6%, n=611) were most common in PN. Regarding the clinical outcomes, 18.7% (n=2,158) finally expired, 58.1% (n=7,027) were admitted to ICU, and the mean hospital days after NT-related complication were 31.3 days. Volume overload (odds ratio [OR]=3.48) and renal abnormality (OR=2.50) were closely associated with hospital death; hyperammonemia (OR=3.09) and renal abnormality (OR=2.77) were associated with ICU admission; “micronutrient and vitamin deficiency” (geometric mean [GM]=2.23) and volume overload (GM=1.61) were associated with a longer hospital stay. Conclusion:NT may induce or be associated with several complications, and some of them may seriously affect the patient’s outcome. NST personnel in each hospital should be aware of each problem during nutritional support. -
Citations
Citations to this article as recorded by  - Provision of Enteral Nutrition in the Surgical Intensive Care Unit: A Multicenter Prospective Observational Study
Chan-Hee Park, Hak-Jae Lee, Suk-Kyung Hong, Yang-Hee Jun, Jeong-Woo Lee, Nak-Jun Choi, Kyu-Hyouck Kyoung
Annals of Clinical Nutrition and Metabolism.2022; 14(2): 66. CrossRef - Pathophysiology and protective approaches of gut injury in critical illness
Chang Yeon Jung, Jung Min Bae
Yeungnam University Journal of Medicine.2021; 38(1): 27. CrossRef - Nutrition Support Team Reconsultation During Nutrition Therapy in Korea
Eun‐Mi Seol, Yun‐Suhk Suh, Dal Lae Ju, Hye Jung Bae, Eunjung Kim, Hyuk‐Joon Lee
Journal of Parenteral and Enteral Nutrition.2021; 45(2): 357. CrossRef
-
986
View
-
6
Download
-
3
Crossref
|