-
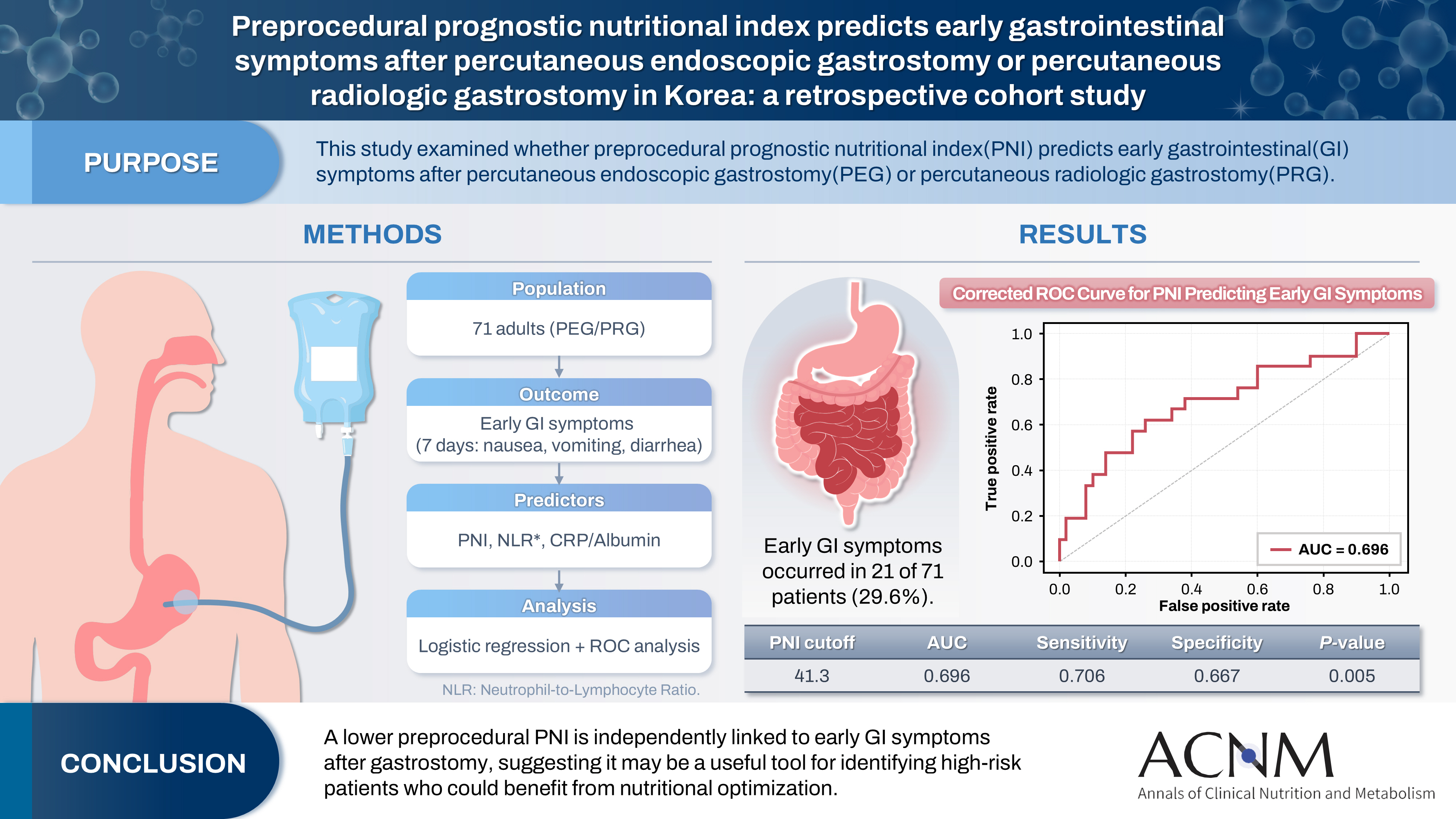
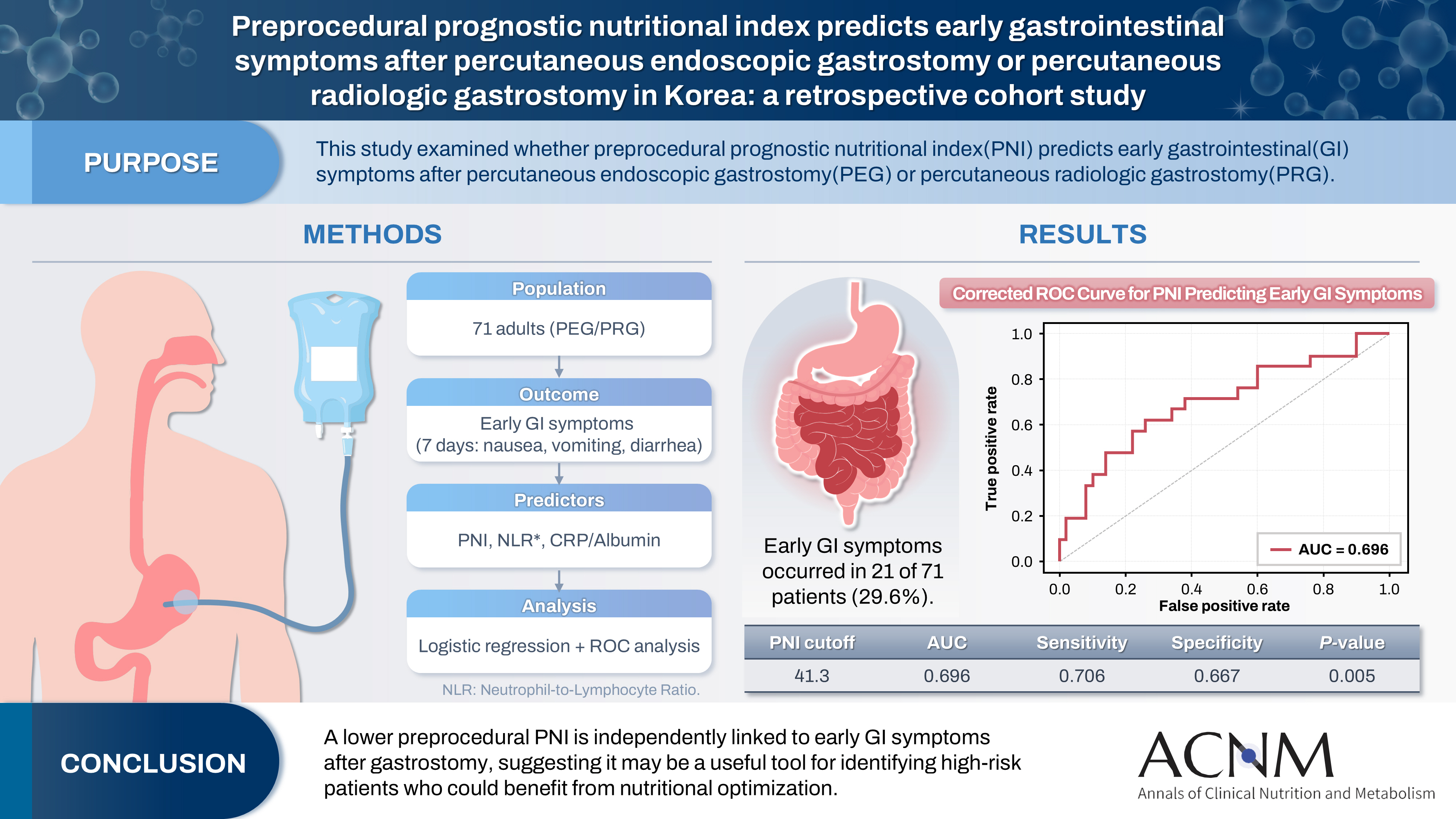
Preprocedural prognostic nutritional index predicts early gastrointestinal symptoms after percutaneous endoscopic gastrostomy or percutaneous radiologic gastrostomy in Korea: a retrospective cohort study
-
Yoonhong Kim, Jee Young Lee, Yeajin Moon, Seung Hun Lee, Kyung Won Seo, Ki Hyun Kim
-
Ann Clin Nutr Metab 2025;17(3):196-202. Published online December 1, 2025
-
DOI: https://doi.org/10.15747/ACNM.25.0032
-
-
 Graphical Abstract Graphical Abstract
 Abstract Abstract
 PDF PDF
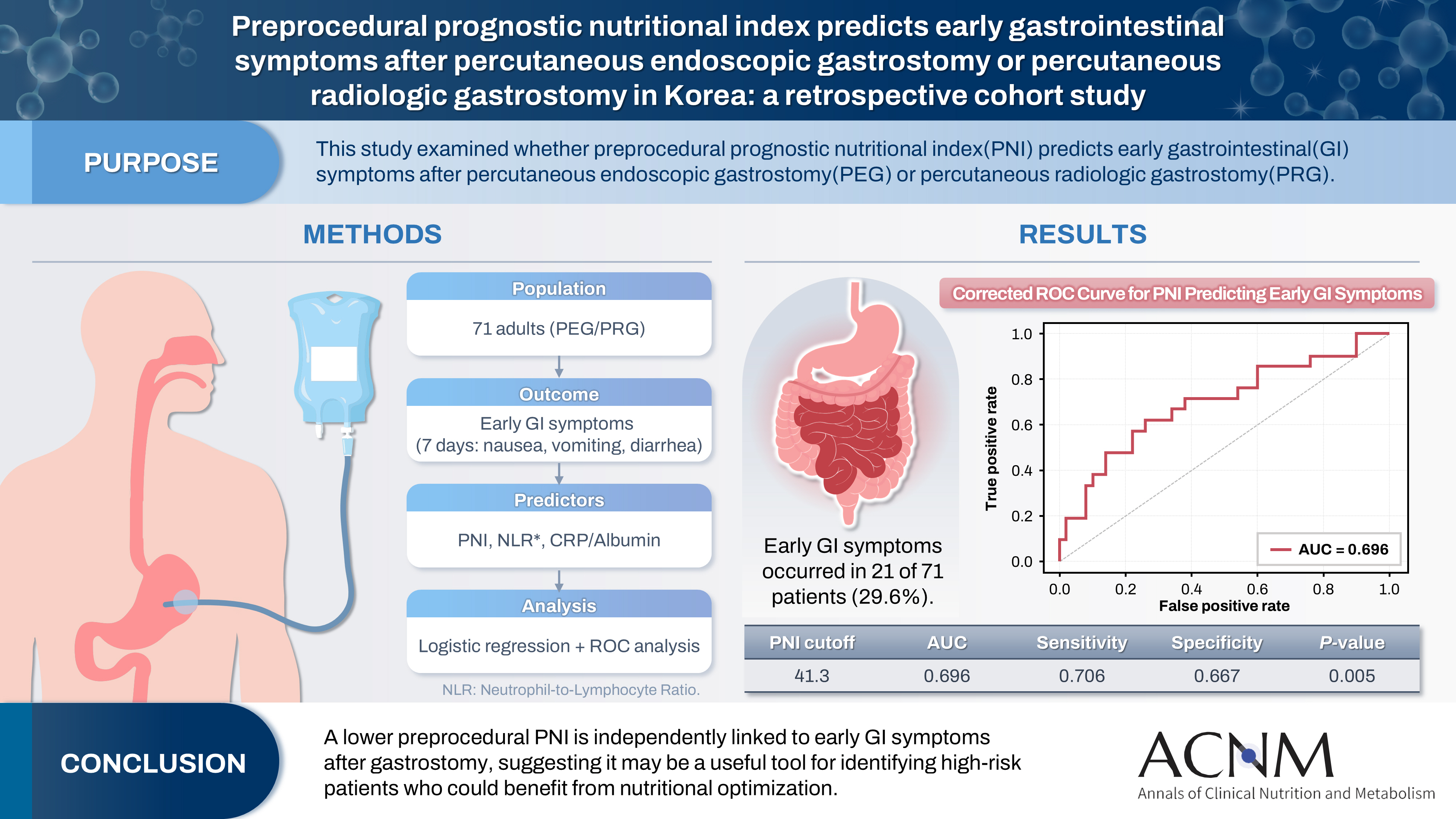 - Purpose
The prognostic nutritional index (PNI) reflects immunonutritional status and is a well-established predictor of surgical outcomes. Although its association with post-gastrostomy mortality has been documented, its relationship with early gastrointestinal (GI) symptoms remains unclear. This study aimed to evaluate whether the preprocedural PNI predicts early GI symptoms following percutaneous gastrostomy, including percutaneous endoscopic gastrostomy (PEG) and percutaneous radiologic gastrostomy (PRG).
Methods
This retrospective study included 71 adults who underwent PEG or PRG. Early GI symptoms, such as nausea, vomiting, and diarrhea, occurring within 7 days were recorded. The preprocedural PNI, neutrophil-to-lymphocyte ratio (NLR), and the C-reactive protein (CRP)-to-albumin ratio were analyzed using logistic regression to identify predictors. Receiver operating characteristic (ROC) analysis was performed to assess the PNI’s discriminative performance.
Results
Early GI symptoms occurred in 21 of 71 patients (29.6%). In univariate analysis, the PNI (P=0.009) and CRP-to-albumin ratio (P=0.018) were significant predictors, whereas NLR was not (P=0.125). After adjustment for potential confounders, including age, sex, body mass index, and NLR, the PNI remained an independent predictor of early GI symptoms (adjusted odds ratio, 0.90; 95% confidence interval, 0.83–0.98; P=0.021). ROC analysis for the PNI produced an area under the curve of 0.696, with an optimal cutoff value of 41.3 (sensitivity 70.6%, specificity 66.7%).
Conclusion
A lower preprocedural PNI is independently associated with the development of early GI symptoms after gastrostomy. The PNI may serve as a practical screening tool to identify high-risk patients who could benefit from preemptive nutritional optimization.
-
Nutritional support for critically ill patients by the Korean Society for Parenteral and Enteral Nutrition — part I: a clinical practice guideline
-
Seung Hwan Lee, Jae Gil Lee, Min Kwan Kwon, Jiyeon Kim, Mina Kim, Jeongyun Park, Jee Young Lee, Ye Won Sung, Bomi Kim, Seong Eun Kim, Ji Yoon Cho, A Young Lim, In Gyu Kwon, Miyoung Choi, KSPEN Guideline Committee
-
Ann Clin Nutr Metab 2024;16(3):89-111. Published online December 1, 2024
-
DOI: https://doi.org/10.15747/ACNM.2024.16.3.89
-
-
 Abstract Abstract
 PDF PDF Supplementary Material Supplementary Material
- Purpose: Nutritional support for adult critically ill patients is essential due to the high risk of malnutrition, which can lead to severe complications. This paper aims to develop evidence-based guidelines to optimize nutritional support in intensive care units (ICUs).
Methods: The Grading Recommendations, Assessment, Development and Evaluation process was used to develop and summarize the evidence on which the recommendations were based. Clinical outcomes were assessed for seven key questions.
Results: We recommend the following: (1) initiate enteral nutrition (EN) within 48 hours after treatment as it is associated with improved outcomes, including reduced infection rates and shorter ICU stays; (2) early EN is preferred over early parenteral nutrition due to better clinical outcomes; (3) the use of supplementary parenteral nutrition to meet energy targets during the first week of ICU admission in patients receiving early EN is conditionally recommended based on patient-specific needs; (4) limited caloric support should be supplied to prevent overfeeding and related complications, particularly in the early phase of critical illness; (5) higher protein intake is suggested to improve clinical outcomes, such as muscle preservation and overall recovery; (6) additional enteral or parenteral glutamine is conditionally recommended against due to the lack of significant benefit and potential harm; and (7) fish oil-containing lipid emulsions is conditionally recommended due to their potential to enhance clinical outcomes, including reduced infection rates and shorter ICU stays.
Conclusion: These evidence-based recommendations can improve clinical outcomes and support healthcare providers in making informed decisions about nutritional interventions in the ICU.
-
Citations
Citations to this article as recorded by  - Enteral Nutrition Versus a Combination of Enteral and Parenteral Nutrition in Critically Ill Adult Patients in the Intensive Care Unit: An Overview of Systematic Reviews and Meta-Analysis
Paraskevi Papanikolaou, Xenophon Theodoridis, Androniki Papaemmanouil, Niki N. Papageorgiou, Alexandra Tsankof, Anna-Bettina Haidich, Christos Savopoulos, Konstantinos Tziomalos
Journal of Clinical Medicine.2025; 14(3): 991. CrossRef
-
22,207
View
-
511
Download
-
1
Crossref
|