Indexed in:
Scopus, KCI, KoreaMed
Scopus, KCI, KoreaMed

Search
- Page Path
- HOME > Search
Guideline
- A practical guide for enteral nutrition from the Korean Society for Parenteral and Enteral Nutrition: Part II. selection and initiation of enteral feeding routes
- Ja Kyung Min, Ye Rim Chang, Bo-Eun Kim, In Seok Lee, Jung Mi Song, Hyunjung Kim, Jae Hak Kim, Kyung Won Seo, Sung Shin Kim, Chi-Min Park, Jeongyun Park, Eunjung Kim, Eunmi Sul, Sung-Sik Han, Jeong Wook Kim, Seungwan Ryu, Minji Seok, Jinhee Yoon, Eunhee Kong, Youn Soo Cho, Jeong Meen Seo, for KSPEN Enteral Nutrition Committee
- Ann Clin Nutr Metab 2025;17(3):165-171. Published online December 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0037
-
 Abstract
Abstract
 PDF
PDF - Purpose
We developed evidence-based recommendations for selecting and initiating the enteral nutrition (EN) delivery route in adult and pediatric patients to improve safety and standardize practice in Korea.
Methods
Key questions covered feeding tube selection, methods to verify tube placement, confirmation in pediatric patients, and timing of EN following percutaneous endoscopic gastrostomy (PEG). Recommendations were drafted and refined through multidisciplinary expert consensus under the Korean Society for Parenteral and Enteral Nutrition (KSPEN).
Results
Feeding tube selection should be based on gastrointestinal anatomy, function, and expected EN duration. Short-term feeding is recommended with nasogastric or orogastric tubes, whereas long-term feeding should use percutaneous or surgical routes such as PEG. Tube position must always be verified before use, preferably with radiography or pH testing; auscultation alone is unreliable and should not be used. In pediatric patients, radiographic confirmation remains the gold standard, although pH testing and insertion-length assessment may be considered when imaging is not feasible. After PEG, EN can be initiated safely within 4 hours in both adults and children without increasing complications if trained staff monitor for leakage or infection.
Conclusion
This guideline offers a structured framework for safe and timely EN tailored to patient characteristics. Early verification and multidisciplinary collaboration help reduce complication, improving outcomes of EN therapy.
- 445 View
- 31 Download

Original Article
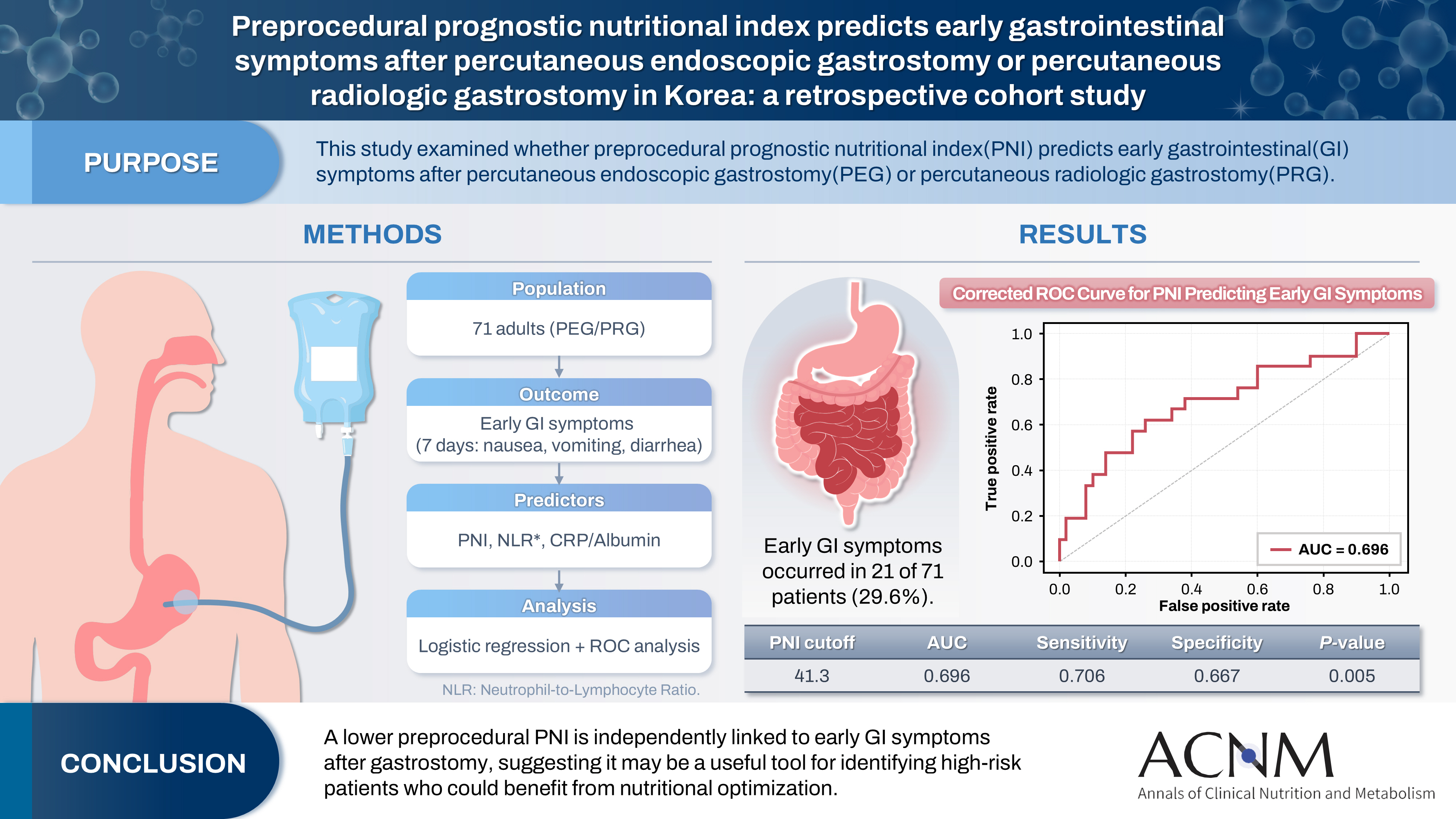
- Preprocedural prognostic nutritional index predicts early gastrointestinal symptoms after percutaneous endoscopic gastrostomy or percutaneous radiologic gastrostomy in Korea: a retrospective cohort study
- Yoonhong Kim, Jee Young Lee, Yeajin Moon, Seung Hun Lee, Kyung Won Seo, Ki Hyun Kim
- Ann Clin Nutr Metab 2025;17(3):196-202. Published online December 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0032
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 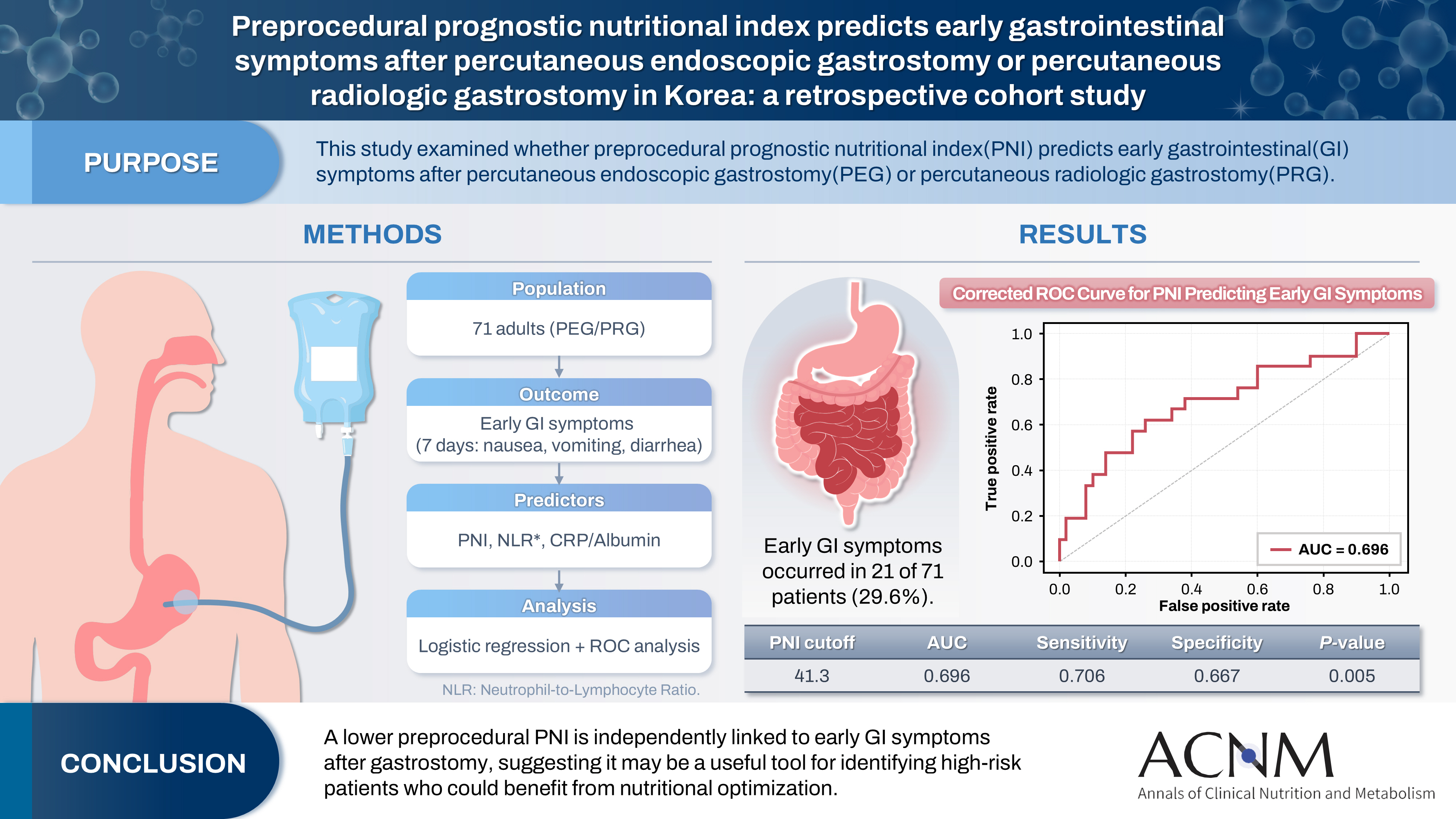
- Purpose
The prognostic nutritional index (PNI) reflects immunonutritional status and is a well-established predictor of surgical outcomes. Although its association with post-gastrostomy mortality has been documented, its relationship with early gastrointestinal (GI) symptoms remains unclear. This study aimed to evaluate whether the preprocedural PNI predicts early GI symptoms following percutaneous gastrostomy, including percutaneous endoscopic gastrostomy (PEG) and percutaneous radiologic gastrostomy (PRG).
Methods
This retrospective study included 71 adults who underwent PEG or PRG. Early GI symptoms, such as nausea, vomiting, and diarrhea, occurring within 7 days were recorded. The preprocedural PNI, neutrophil-to-lymphocyte ratio (NLR), and the C-reactive protein (CRP)-to-albumin ratio were analyzed using logistic regression to identify predictors. Receiver operating characteristic (ROC) analysis was performed to assess the PNI’s discriminative performance.
Results
Early GI symptoms occurred in 21 of 71 patients (29.6%). In univariate analysis, the PNI (P=0.009) and CRP-to-albumin ratio (P=0.018) were significant predictors, whereas NLR was not (P=0.125). After adjustment for potential confounders, including age, sex, body mass index, and NLR, the PNI remained an independent predictor of early GI symptoms (adjusted odds ratio, 0.90; 95% confidence interval, 0.83–0.98; P=0.021). ROC analysis for the PNI produced an area under the curve of 0.696, with an optimal cutoff value of 41.3 (sensitivity 70.6%, specificity 66.7%).
Conclusion
A lower preprocedural PNI is independently associated with the development of early GI symptoms after gastrostomy. The PNI may serve as a practical screening tool to identify high-risk patients who could benefit from preemptive nutritional optimization.
- 697 View
- 15 Download

Review Article
- Selection of the Enterostomy Feeding Route in Enteral Nutrition
- Dong-Seok Han
- Ann Clin Nutr Metab 2022;14(2):50-54. Published online December 1, 2022
- DOI: https://doi.org/10.15747/ACNM.2022.14.2.50
-
 Abstract
Abstract
 PDF
PDF - Enteral nutrition has several physiologic advantages. For example, it can reduce complications, result in immunological improvement, and prevent bacterial translocation by maintaining the integrity of the intestinal barrier. Enteral tube feeding has a major role in nutritional support of patients with swallowing disorders caused by stroke or other neurologic disorders, neoplasms of the upper digestive tract, and benign esophageal stricture. This review article aimed to present the current knowledge on the clinical application of enteral tube feeding. Especially, based on a literature search on PubMed using the index terms of enteral tube feeding; the indications, advantages, and disadvantages; and insertion methods of various enteral tubes were identified.
-
Citations
Citations to this article as recorded by- Preprocedural prognostic nutritional index predicts early gastrointestinal symptoms after percutaneous endoscopic gastrostomy or percutaneous radiologic gastrostomy in Korea: a retrospective cohort study
Yoonhong Kim, Jee Young Lee, Yeajin Moon, Seung Hun Lee, Kyung Won Seo, Ki Hyun Kim
Ann Clin Nutr Metab.2025; 17(3): 196. CrossRef
- Preprocedural prognostic nutritional index predicts early gastrointestinal symptoms after percutaneous endoscopic gastrostomy or percutaneous radiologic gastrostomy in Korea: a retrospective cohort study
- 6,607 View
- 44 Download
- 1 Crossref

Original Article
- The Utility of Open Gastrostomy Using Local Anesthesia and a Gastrostomy Tube for Percutaneous Endoscopic Gastrostomy
- Jae Kyun Park, Chang In Choi, Dae Hwan Kim
- Surg Metab Nutr 2020;11(1):22-26. Published online June 30, 2020
- DOI: https://doi.org/10.18858/smn.2020.11.1.22
-
 Abstract
Abstract
 PDF
PDF - Purpose: The purpose of this study is to introduce the technical details of open gastrostomy using local anesthesia and a gastrostomy tube for percutaneous endoscopic gastrostomy, and to evaluate the safety and utility of the procedure.
Materials and Methods: Between January 2011 and December 2015, a total of 46 patients who underwent open gastrostomy using local anesthesia and a gastrostomy tube for percutaneous endoscopic gastrostomy (open group, n=25) or laparoscopic gastrostomy (laparoscopy group, n=21) were enrolled in this retrospective study. We analyzed the clinical data and the perioperative data.
Results: There were no significant differences in the clinical characteristics of the two groups. However, the patients with a high anesthetic risk (American Society of Anesthesiologists [ASA] grade 3 or more) were significantly more prevalent in the open group than in the laparoscopic group (96.0% vs. 66.7%, respectively, P=0.013). The operation time (31.8±6.6 vs. 67.9±15.7 minutes, respectively, P<0.001) and the time to first tubal feeding (1.3±0.6 vs. 2.7±1.3 days, respectively, P<0.001) was significantly shorter in the open group than that in the laparoscopic group. Postoperative complications were more frequent in the laparoscopic group (4 cases, 19%) than that in the open group (1 case, 4%), but there was no statistically significant difference.
Conclusion: Open gastrostomy using local anesthesia and a gastrostomy tube for PEG is a safe and feasible method for treating patients with a high anesthetic risk.
- 762 View
- 2 Download


 E-submission
E-submission KSPEN
KSPEN KSSMN
KSSMN ASSMN
ASSMN JSSMN
JSSMN
 First
First Prev
Prev


