Articles
- Page Path
- HOME > Ann Clin Nutr Metab > Volume 16(2); 2024 > Article
- Review Definition, assessments, and current research on sarcopenia in children: a narrative review
-
Min-Jung Bang

-
Annals of Clinical Nutrition and Metabolism 2024;16(2):49-56.
DOI: https://doi.org/10.15747/ACNM.2024.16.2.49
Published online: August 1, 2024
Division of Pediatric Surgery, Department of Surgery, Ajou University School of Medicine, Suwon, Korea
- Corresponding author: Min-Jung Bang, email: ventvertb@gmail.com
© 2024 The Korean Society of Surgical Metabolism and Nutrition · The Korean Society for Parenteral and Enteral Nutrition
This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0), which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 222 Views
- 7 Download
Abstract
-
Purpose Sarcopenia is a well-established prognostic factor for the clinical outcomes of adult patients with cancer and chronic diseases and correlates with increased intensive care unit admissions and prolonged hospital stays. However, research on sarcopenia in children is limited due to its undefined criteria and a lack of studies exploring its impact on clinical outcomes.
-
Current concept The challenges in pediatric sarcopenia research include the absence of standardized body composition methods to quantify muscle mass and muscular function, as well as inconsistencies in definitions. Additionally, there is a lack of age- and gender-specific normative data, particularly for young children and infants. Most studies also lack assessments of muscle function, which can lead to bias and misclassification of sarcopenia. The field is further hindered by poor study quality, limited outcome-focused research, and a dearth of longitudinal data. While some studies suggest that various diseases can affect children’s lean muscle mass, few have linked changes in muscle mass to clinical outcomes.
-
Conclusion The existing literature on pediatric sarcopenia and its relationship with medical and surgical outcomes is sparse and indicates poorer outcomes associated with sarcopenia. Although extensive research has established a link between sarcopenia and adverse outcomes in adults, information on its impact in pediatric populations remains scarce. Further studies are needed to elucidate the association between muscle mass and outcomes in pediatric surgical patients.
Introduction
Definition and pathophysiology of sarcopenia
Pediatric sarcopenia and surgery
Conclusion
Supplementary materials
Acknowledgments
Conflict of interest
The author of this manuscript has no conflicts of interest to disclose.
Funding
None.
Data availability
None.
| Reference | Population | Study design | Sample size (n) | Age (yr) | Methodology or modality | Indicators of muscle mass | Indicators of muscle strength or function | Definition of sarcopenia | Clinical outcome |
|---|---|---|---|---|---|---|---|---|---|
| Dedhia et al., 2018 [17] | Pediatric patients with UC undergoing colectomy | Retrospective | 29 | Range: 13–18 |
MRI L3 |
PSMA and PMA | None | Lowest tertile of PSMA | 62% of patients with post colectomy complications with ulcerative colitis have significantly reduced PSMA |
| López et al., 2017 [30] | Pediatric patients with perforated appendicitis | Retrospective | 36 | Median: 11 |
CT (pre and post op), L3 |
PMA | None | Mean percentage change in PMA index (PMA/height2) |
N/A (Pediatric patients with complex appendicitis experience sarcopenic changes during hospital admission) |
| Mager et al., 2018 [19] | Pediatric post-LT patients | Retrospective | 41 | Range: 0.5–17 | DXA | SMM-z | None | SMM-z <–2SD of age and gender normative values | Sarcopenia was significantly associated with increased hospitalization and ventilator dependency |
| Oh et al., 2019 [26] | Pediatric patients undergoing the Fontan operation | Retrospective | 74 | Range: 2.8–3.3 |
CT (pre and post op) |
Bilateral pectoralis muscles (T2) and erector spinae muscles (T12) | None | None | Preoperative low muscle mass was associated with poor early postoperative outcomes in pediatric patients undergoing the Fontan operation |
| Takeda et al., 2021 [25] | Children with LTfor biliary atresia | Retrospective | 89 | Range: 0.6–0.7 |
CT (pre and post op) L3 and L4 |
PMA | None | tPMA-z<–2 | Sarcopenia in infants with BA may be associated with patient survival and serve as an effective marker for post-operative outcomes of LT |
| Ritz et al., 2021 [15] | Children with hepato-blastoma | Retrospective | 33 | Range: 1.2–3.0 |
CT and MRI L3–L4 and L4–L5 |
PMA | None | tPMA-z<–2 | Sarcopenia was an additional risk factor for relapse in children with high-risk HB |
| Raghu et al., 2022 [27] | Pediatric intestinal transplant recipient | Retrospective | 56 | Range: 1.8–9.8 |
CT L3–L4 and L4–L5 |
PMA | None | tPMA-z<–2 |
N/A (Sarcopenia was not associated with decreased graft survival) |
| Muñoz-Serrano et al., 2023 [28] | Children with hepato-blastoma | Retrospective | 21 | Median: 3 | MRI | PMA | None | tPMA-z<–2 |
N/A (Sarcopenia at diagnosis was associated with higher rates of metastases and surgical complications) |
| Jang et al., 2023 [29] | Pediatric patients undergoing total correction of TOF | Retrospective | 330 | Mean: 5 | Chest CT(pre and post op) | Bilateral pectoralis muscles (T2) and erector spinae muscles (T12) | None | MMI-z<–2 |
N/A (Preoperative sarcopenia did not predict early postoperative major adverse events) |
UC = ulcerative colitis; LT = liver transplantation; TOF = tetralogy of Fallot; MRI = magnetic resonance imaging; CT = computed tomography; op = operative; DXA = dual-energy X-ray absorptiometry; PSMA = paraspinous muscle area; PMA = psoas muscle area; SMM-z = skeletal muscle mass z-score; SD = standard deviation; tPMA-z = total psoas muscle area z-score; N/A = not assessed; BA = biliary atresia; HB = hepatoblastoma.
- 1. Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, et al. Sarcopenia: European consensus on definition and diagnosis: report of the European Working Group on Sarcopenia in Older People. Age Ageing 2010;39:412-23. PubMedPMC
- 2. Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing 2019;48:16-31. ArticlePubMedPDF
- 3. Thomas DR. Loss of skeletal muscle mass in aging: examining the relationship of starvation, sarcopenia and cachexia. Clin Nutr 2007;26:389-99. ArticlePubMed
- 4. Triarico S, Rinninella E, Mele MC, Cintoni M, Attinà G, Ruggiero A. Prognostic impact of sarcopenia in children with cancer: a focus on the psoas muscle area (PMA) imaging in the clinical practice. Eur J Clin Nutr 2022;76:783-8. ArticlePubMedPDF
- 5. Jung HN, Jung CH, Hwang YC. Sarcopenia in youth. Metabolism 2023;144:155557. ArticlePubMed
- 6. Mager DR, Hager A, Gilmour S. 2023;Challenges and physiological implications of sarcopenia in children and youth in health and disease. Curr Opin Clin Nutr Metab Care 26:528-33. ArticlePubMed
- 7. Ooi PH, Thompson-Hodgetts S, Pritchard-Wiart L, Gilmour SM, Mager DR. Pediatric sarcopenia: a paradigm in the overall definition of malnutrition in children? JPEN J Parenter Enteral Nutr 2020;44:407-18. ArticlePubMedPDF
- 8. Mager DR, Hager A, Ooi PH, Siminoski K, Gilmour SM, Yap JYK. Persistence of sarcopenia after pediatric liver transplantation is associated with poorer growth and recurrent hospital admissions. JPEN J Parenter Enteral Nutr 2019;43:271-80. ArticlePubMedPDF
- 9. Mangus RS, Bush WJ, Miller C, Kubal CA. Severe sarcopenia and increased fat stores in pediatric patients with liver, kidney, or intestine failure. J Pediatr Gastroenterol Nutr 2017;65:579-83. ArticlePubMed
- 10. Lurz E, Patel H, Frimpong RG, Ricciuto A, Kehar M, Wales PW, et al. Sarcopenia in children with end-stage liver disease. J Pediatr Gastroenterol Nutr 2018;66:222-6. ArticlePubMed
- 11. Rezende IFB, Conceição-Machado MEP, Souza VS, Santos EMD, Silva LR. Sarcopenia in children and adolescents with chronic liver disease. J Pediatr (Rio J) 2020;96:439-46. ArticlePubMed
- 12. Kawakubo N, Kinoshita Y, Souzaki R, Koga Y, Oba U, Ohga S, et al. The Influence of sarcopenia on high-risk neuroblastoma. J Surg Res 2019;236:101-5. ArticlePubMed
- 13. Suzuki D, Kobayashi R, Sano H, Hori D, Kobayashi K. Sarcopenia after induction therapy in childhood acute lymphoblastic leukemia: its clinical significance. Int J Hematol 2018;107:486-9. ArticlePubMedPDF
- 14. Amini B, Boyle SP, Boutin RD, Lenchik L. Approaches to assessment of muscle mass and myosteatosis on computed tomography: a systematic review. J Gerontol A Biol Sci Med Sci 2019;74:1671-8. ArticlePubMedPMCPDF
- 15. Ritz A, Kolorz J, Hubertus J, Ley-Zaporozhan J, von Schweinitz D, Koletzko S, et al. Sarcopenia is a prognostic outcome marker in children with high-risk hepatoblastoma. Pediatr Blood Cancer 2021;68:e28862. ArticlePubMedPDF
- 16. Lurz E, Patel H, Lebovic G, Quammie C, Woolfson JP, Perez M, et al. 2020;Paediatric reference values for total psoas muscle area. J Cachexia Sarcopenia Muscle 11:405-14. ArticlePubMedPMCPDF
- 17. Dedhia PH, White Y, Dillman JR, Adler J, Jarboe MD, Teitelbaum DH, et al. Reduced paraspinous muscle area is associated with post-colectomy complications in children with ulcerative colitis. J Pediatr Surg 2018;53:477-82. ArticlePubMed
- 18. Atlan L, Cohen S, Shiran S, Sira LB, Pratt LT, Yerushalmy-Feler A. Sarcopenia is a predictor for adverse clinical outcome in pediatric inflammatory bowel disease. J Pediatr Gastroenterol Nutr 2021;72:883-8. ArticlePubMed
- 19. Mager DR, Carroll MW, Wine E, Siminoski K, MacDonald K, Kluthe CL, et al. Vitamin D status and risk for sarcopenia in youth with inflammatory bowel diseases. Eur J Clin Nutr 2018;72:623-6. ArticlePubMedPDF
- 20. Davies A, Nixon A, Muhammed R, Tsintzas K, Kirkham S, Stephens FB, et al. Reduced skeletal muscle protein balance in paediatric Crohn's disease. Clin Nutr 2020;39:1250-7. ArticlePubMed
- 21. Rayar M, Webber CE, Nayiager T, Sala A, Barr RD. Sarcopenia in children with acute lymphoblastic leukemia. J Pediatr Hematol Oncol 2013;35:98-102. ArticlePubMed
- 22. Mueske NM, Mittelman SD, Wren TAL, Gilsanz V, Orgel E. Myosteatosis in adolescents and young adults treated for acute lymphoblastic leukemia. Leuk Lymphoma 2019;60:3146-53. ArticlePubMedPMC
- 23. Alonso EM, Ye W, Hawthorne K, Venkat V, Loomes KM, Mack CL, et al. Impact of steroid therapy on early growth in infants with biliary atresia: the multicenter steroids in biliary atresia randomized trial. J Pediatr 2018;202:179-85.e4. ArticlePubMedPMC
- 24. Woolfson JP, Perez M, Chavhan GB, Johara FT, Lurz E, Kamath BM, et al. Sarcopenia in children with end-stage liver disease on the transplant waiting list. Liver Transpl 2021;27:641-51. ArticlePubMedPMCPDF
- 25. Takeda M, Sakamoto S, Uchida H, Shimizu S, Yanagi Y, Fukuda A, et al. Impact of sarcopenia in infants with liver transplantation for biliary atresia. Pediatr Transplant 2021;25:e13950. ArticlePubMedPDF
- 26. Oh J, Shin WJ, Jeong D, Yun TJ, Park CS, Choi ES, et al. 2019;Low muscle mass as a prognostic factor for early postoperative outcomes in pediatric patients undergoing the fontan operation: a retrospective cohort study. J Clin Med 8:1257.ArticlePubMedPMC
- 27. Raghu VK, Sico R, Rudolph JA, Mazariegos GV, Squires J, Squires JE. Sarcopenia prevalence in pediatric intestinal transplant recipients: Implications on post-transplant outcomes. Pediatr Transplant 2022;26:e14256. ArticlePubMedPDF
- 28. Muñoz-Serrano AJ, Estefanía-Fernández K, Oterino C, Ramírez-Amoros C, Navarro G, Sastre A, et al. 2023;Sarcopenia as a prognostic factor in patients with hepatoblastoma: does it influence surgical outcomes and survival? Preliminary retrospective study. J Pediatr Surg 58:2149-55. ArticlePubMed
- 29. Jang HY, Shin WJ, Jeong D, Baek J, Song IK. Association between preoperative sarcopenia and early postoperative outcomes in pediatric patients undergoing total correction of tetralogy of fallot: a retrospective cohort study. J Cardiothorac Vasc Anesth 2023;37:2020-6. ArticlePubMed
- 30. López JJ, Cooper JN, Albert B, Adler B, King D, Minneci PC. Sarcopenia in children with perforated appendicitis. J Surg Res 2017;220:1-5. ArticlePubMed
- 31. Burrows R, Correa-Burrows P, Reyes M, Blanco E, Albala C, Gahagan S. Low muscle mass is associated with cardiometabolic risk regardless of nutritional status in adolescents: a cross-sectional study in a chilean birth cohort. Pediatr Diabetes 2017;18:895-902. ArticlePubMedPMCPDF
- 32. Kim JH, Park YS. Low muscle mass is associated with metabolic syndrome in Korean adolescents: the Korea National Health and Nutrition Examination Survey 2009-2011. Nutr Res 2016;36:1423-8. ArticlePubMed
References
Figure & Data
REFERENCES
Citations

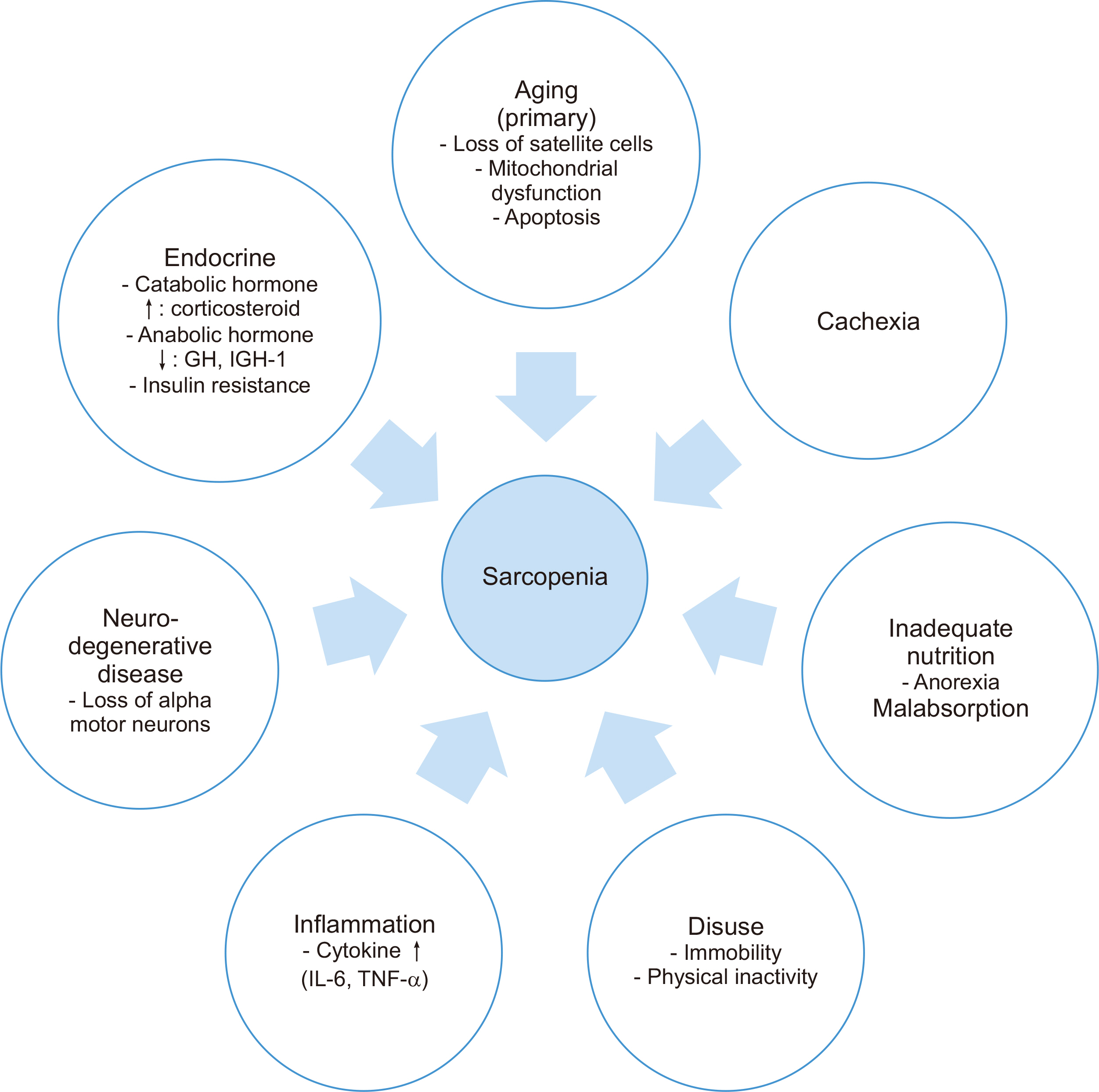
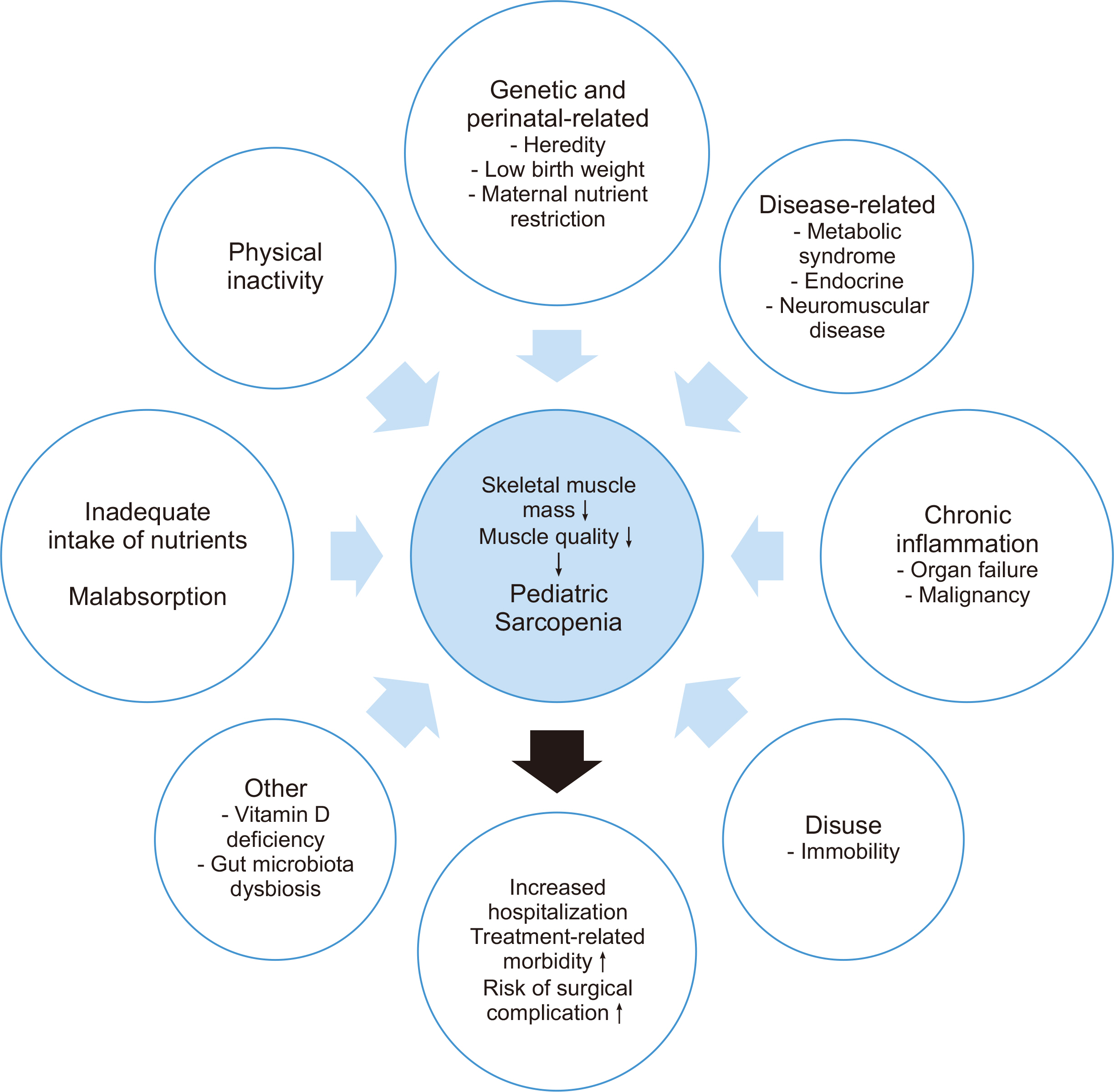
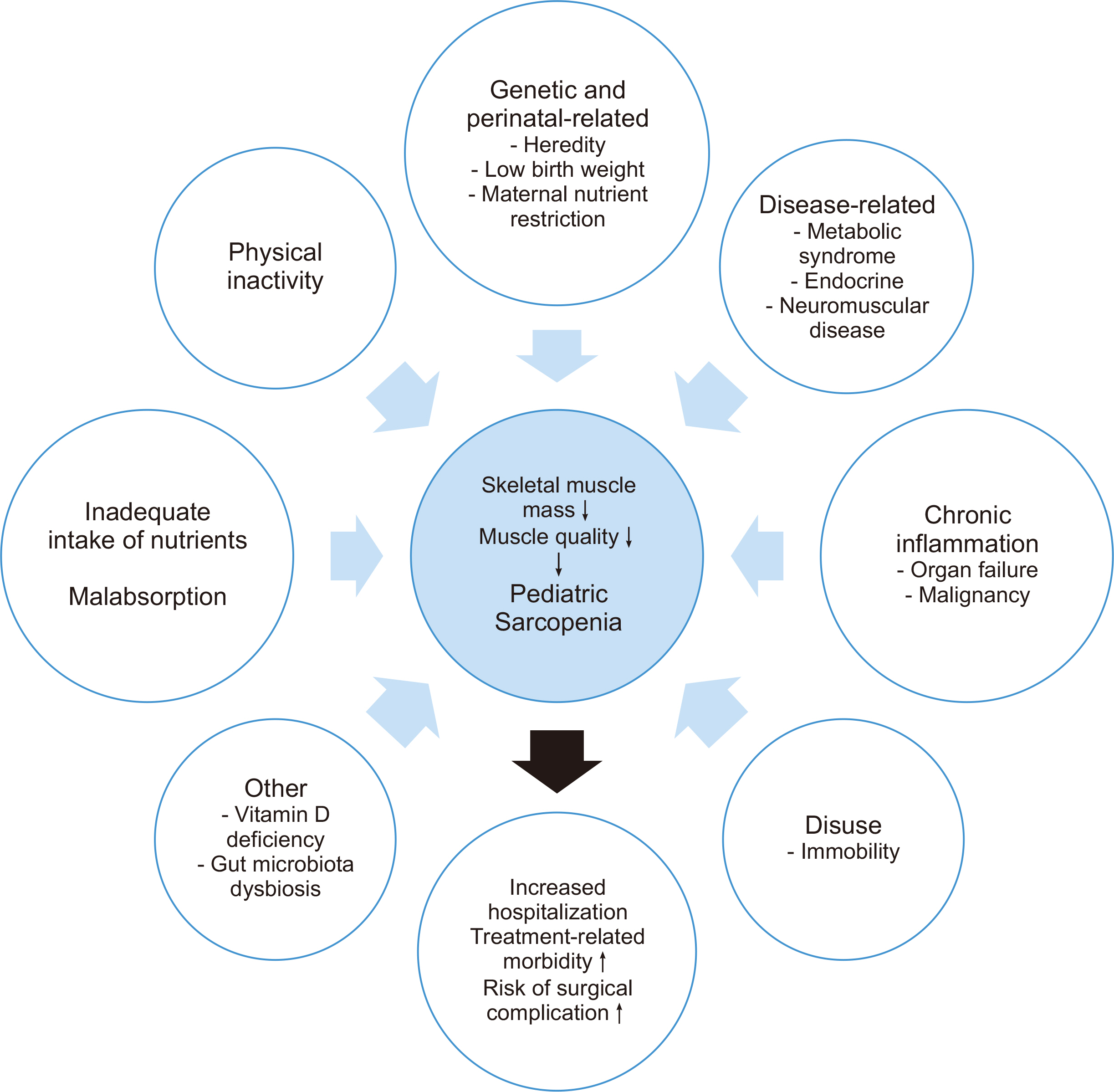
Fig. 1
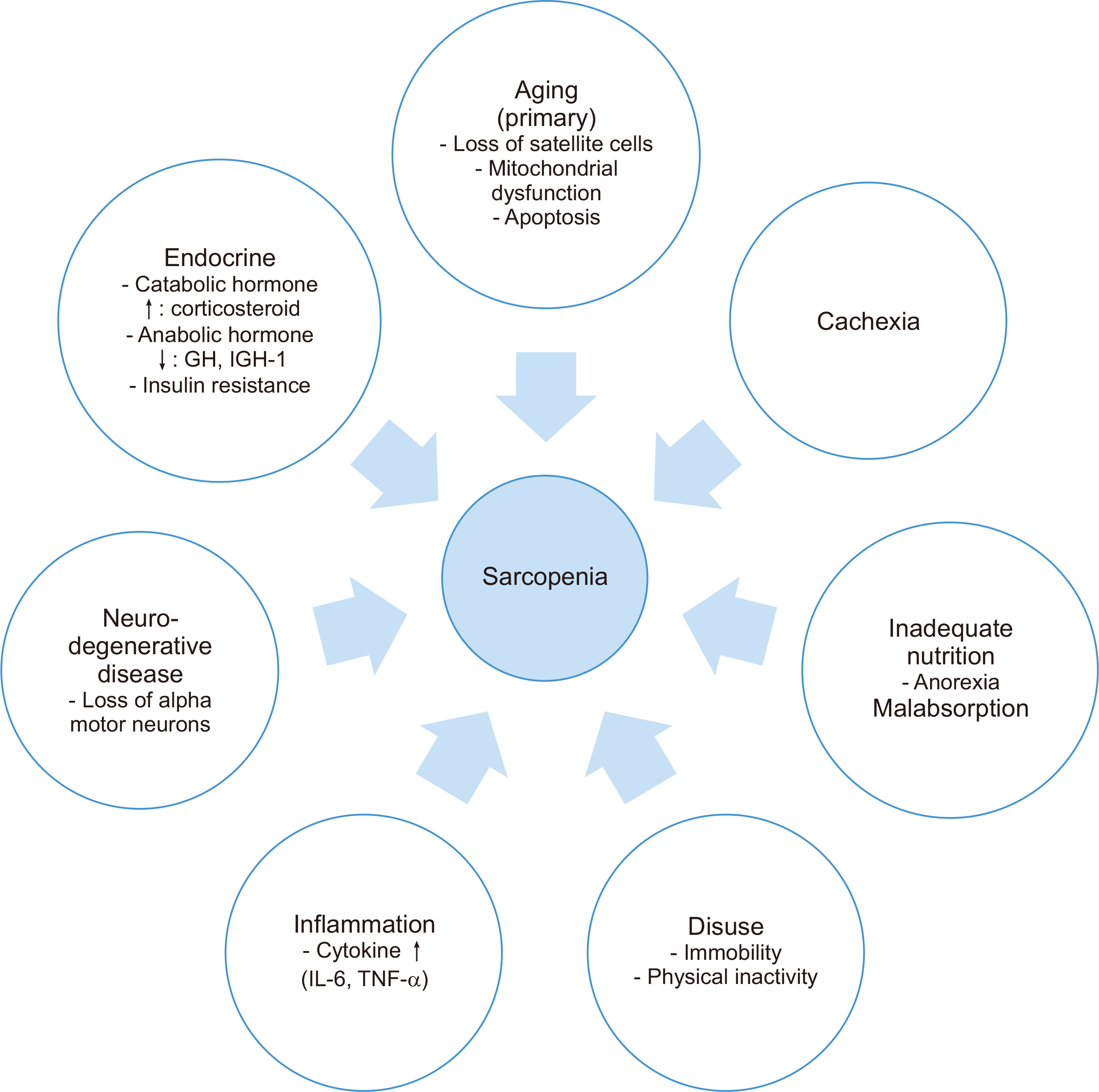
Fig. 2
The 2018 operational definition of sarcopenia (EWGSOP2)
| Criteria | Diagnosis |
|---|---|
| (1) Low muscle strength | Probable sarcopenia is identified by Criterion (1) |
| (2) Low muscle quantity or quality | Diagnosis is confirmed by additional documentation of Criterion (2) |
| (3) Low physical performance | If Criteria (1), (2) and (3) are all met, sarcopenia is considered severe |
Summary of current research on pediatric surgical patients with sarcopenia
| Reference | Population | Study design | Sample size (n) | Age (yr) | Methodology or modality | Indicators of muscle mass | Indicators of muscle strength or function | Definition of sarcopenia | Clinical outcome |
|---|---|---|---|---|---|---|---|---|---|
| Dedhia et al., 2018 [ |
Pediatric patients with UC undergoing colectomy | Retrospective | 29 | Range: 13–18 | MRI L3 |
PSMA and PMA | None | Lowest tertile of PSMA | 62% of patients with post colectomy complications with ulcerative colitis have significantly reduced PSMA |
| López et al., 2017 [ |
Pediatric patients with perforated appendicitis | Retrospective | 36 | Median: 11 | CT (pre and post op), L3 |
PMA | None | Mean percentage change in PMA index (PMA/height2) | N/A (Pediatric patients with complex appendicitis experience sarcopenic changes during hospital admission) |
| Mager et al., 2018 [ |
Pediatric post-LT patients | Retrospective | 41 | Range: 0.5–17 | DXA | SMM-z | None | SMM-z <–2SD of age and gender normative values | Sarcopenia was significantly associated with increased hospitalization and ventilator dependency |
| Oh et al., 2019 [ |
Pediatric patients undergoing the Fontan operation | Retrospective | 74 | Range: 2.8–3.3 | CT (pre and post op) |
Bilateral pectoralis muscles (T2) and erector spinae muscles (T12) | None | None | Preoperative low muscle mass was associated with poor early postoperative outcomes in pediatric patients undergoing the Fontan operation |
| Takeda et al., 2021 [ |
Children with LTfor biliary atresia | Retrospective | 89 | Range: 0.6–0.7 | CT (pre and post op) L3 and L4 |
PMA | None | tPMA-z<–2 | Sarcopenia in infants with BA may be associated with patient survival and serve as an effective marker for post-operative outcomes of LT |
| Ritz et al., 2021 [ |
Children with hepato-blastoma | Retrospective | 33 | Range: 1.2–3.0 | CT and MRI L3–L4 and L4–L5 |
PMA | None | tPMA-z<–2 | Sarcopenia was an additional risk factor for relapse in children with high-risk HB |
| Raghu et al., 2022 [ |
Pediatric intestinal transplant recipient | Retrospective | 56 | Range: 1.8–9.8 | CT L3–L4 and L4–L5 |
PMA | None | tPMA-z<–2 | N/A (Sarcopenia was not associated with decreased graft survival) |
| Muñoz-Serrano et al., 2023 [ |
Children with hepato-blastoma | Retrospective | 21 | Median: 3 | MRI | PMA | None | tPMA-z<–2 | N/A (Sarcopenia at diagnosis was associated with higher rates of metastases and surgical complications) |
| Jang et al., 2023 [ |
Pediatric patients undergoing total correction of TOF | Retrospective | 330 | Mean: 5 | Chest CT(pre and post op) | Bilateral pectoralis muscles (T2) and erector spinae muscles (T12) | None | MMI-z<–2 | N/A (Preoperative sarcopenia did not predict early postoperative major adverse events) |
UC = ulcerative colitis; LT = liver transplantation; TOF = tetralogy of Fallot; MRI = magnetic resonance imaging; CT = computed tomography; op = operative; DXA = dual-energy X-ray absorptiometry; PSMA = paraspinous muscle area; PMA = psoas muscle area; SMM-z = skeletal muscle mass z-score; SD = standard deviation; tPMA-z = total psoas muscle area z-score; N/A = not assessed; BA = biliary atresia; HB = hepatoblastoma.
UC = ulcerative colitis; LT = liver transplantation; TOF = tetralogy of Fallot; MRI = magnetic resonance imaging; CT = computed tomography; op = operative; DXA = dual-energy X-ray absorptiometry; PSMA = paraspinous muscle area; PMA = psoas muscle area; SMM-z = skeletal muscle mass z-score; SD = standard deviation; tPMA-z = total psoas muscle area z-score; N/A = not assessed; BA = biliary atresia; HB = hepatoblastoma.

 KSPEN
KSPEN KSSMN
KSSMN ASSMN
ASSMN
 ePub Link
ePub Link Cite
Cite

