Abstract
-
Purpose
This study aimed to evaluate the current practices, activities, and challenges of nutrition support teams (NSTs) in Korea. The assessment was conducted as part of the 4th NST Leadership Program of the Korean Society of Surgical Metabolism and Nutrition held in 2025, which seeks to foster leadership and enhance team functionality.
-
Methods
A nationwide survey was conducted in February 2025 among 54 NST members from 44 institutions. The survey explored team composition, consultation volume, educational programs, barriers to implementation, institutional support, and reimbursement challenges.
-
Results
Of the 44 participating hospitals, most (86.4%) operated a single NST, with multidisciplinary physician involvement from over three specialties in 77.2% of cases. Inpatient referrals to NSTs were generally low, with less than 10% at 63% of institutions. Only 40.9% had an individual office, and formal incentive systems were reported in 18.1% of hospitals. Educational programs for in-hospital staff were limited (29.5%), and less than half conducted regular academic meetings. Rates of adoption of NST recommendations varied widely, with barriers including a lack of engagement from attending physicians, failure to review the recommendations, and department-specific clinical policies. Efforts to promote NST activation included computerized prescription systems, automated referral workflows, staff education, and quality improvement initiatives. Participants focused on sharing effective NST cases, building incentives, exchanging clinical insights, clarifying team roles and leadership, and developing unified practice guidelines.
-
Conclusion
NSTs in Korea are well established but face ongoing challenges in collaboration and sustainability. Continued leadership and policy support are crucial for enhancing team performance and improving patient outcomes.
-
Keywords: Nutritional support; Nutrition therapy; Quality improvement; Referral and consultation; Reimbursement health insurance
Introduction
Background
In Korea, malnutrition is identified in approximately 20.2% of hospitalized patients and is significantly associated with poorer clinical outcomes [
1]. Since the implementation of the nutrition support team (NST) reimbursement in 2014, multidisciplinary nutritional support has demonstrated clinical benefits and has gained growing institutional recognition. Although reimbursement rates have gradually increased each year, forming and sustaining effective NSTs is still challenged by limited physician engagement, shortages of pharmacists and clinical dietitians facing high workloads, and difficulties in recruiting and retaining nutrition support nurses. Despite clear evidence of improved clinical outcomes, many teams continue to be undervalued and face obstacles to long-term sustainability. To cultivate leadership and enhance team function, the Korean Society of Surgical Metabolism and Nutrition (KSSMN) has organized an annual NST Leadership Program. In 2025, the 4th edition of the program broadened participation to include not only team leaders but also NST members from various hospitals. As part of this initiative, a nationwide survey was conducted to evaluate the current status and challenges experienced by hospital-based NSTs in Korea.
Nearly a decade after the adoption of NST reimbursement, this survey aims to reassess the current landscape, identify persistent barriers, and compare recent findings with previous nationwide studies. Based on these insights, we suggest directions for future policy and improvement strategies.
Methods
Ethics statement
This study received approval from the Institutional Review Board of Busan Paik Hospital, Inje University (IRB No. BPIRB 2025-06-040).
Study design
It is a multicenter, cross-sectional, descriptive study based on survey results. It was described by the STROBE statement [
2].
The survey questionnaires were distributed to 187 of NST leaders and team members in 90 institutions via email, and the author collected the responses in February 2025.
Participants
Before the 4th NST Leadership Program in 2025, the survey was distributed by email to NST leaders and team members across Korean hospitals, including physicians, pharmacists, clinical dietitians, and nurses. Additional responses were obtained on-site during the program.
Variables
The 23 items in the survey form were outcome variables. The survey, developed by the NST Management Committee of KSSMN, included 23 items distributed across six domains: (1) institutional characteristics; (2) NST composition and activities; (3) nutritional screening practices; (4) acceptance and implementation of NST recommendations; (5) reimbursement-related issues; and (6) suggestions for future development. The questionnaire comprised both closed-ended and open-ended items to capture both quantitative trends and qualitative insights (
Supplement 1).
For data analysis, only anonymized responses were provided to the investigators. Responses related to institutions were curated to eliminate duplication, while questions reflecting individual perspectives were included in the dataset without modification. The measurement tool (survey questionnaire) was initially developed by the author and subsequently validated by other board members of the Korean Society of Parenteral and Enteral Nutrition. No reliability test was conducted due to the structure of the questionnaire items, which included binary form, Likert scale, descriptive form, and open-ended questions.
Bias
Since only responses from those who voluntarily participated in this survey are analyzed, it cannot represent the whole opinion of the target people.
Study size
The sample size was not estimated, as this was a descriptive study based on responses from all voluntary participants.
Statistical methods
As the primary objective was descriptive, no inferential statistical analyses were conducted; results are reported as frequency and percentage distributions.
Results
Participants
A total of 54 responses were collected from 44 institutions. When two or more people were answered by an institution, the answer to the current state of the institution was treated as one after confirming the same value, and questions about individuals were reflected as they were.
Basic characteristics of participating institutions
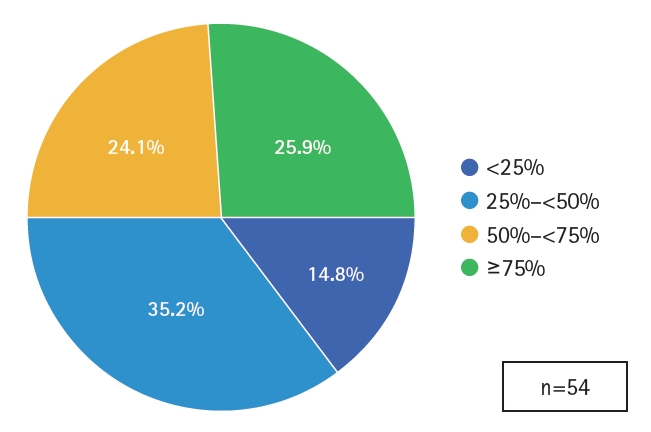
Institutions from across the country participated, including 10 from Seoul (22.7%), six from Gyeonggi (13.6%), and four each from Busan, Daegu, Incheon, Gwangju, and Chungcheong. Daejeon, Gyeongsang, and Jeolla each contributed two responses, while Gangwon and Jeju each had one responding institution. The majority of responses came from hospitals with 501 to 1,000 beds (n=28, 63.6%), followed by institutions with 1,001 to 1,500 beds (n=6, 13.6%). Eight institutions reported bed capacities ranging from 200 to 500, and two responses were from hospitals with more than 1,500 beds (
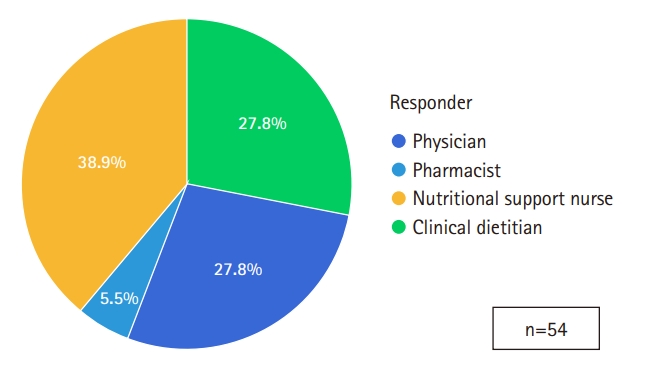
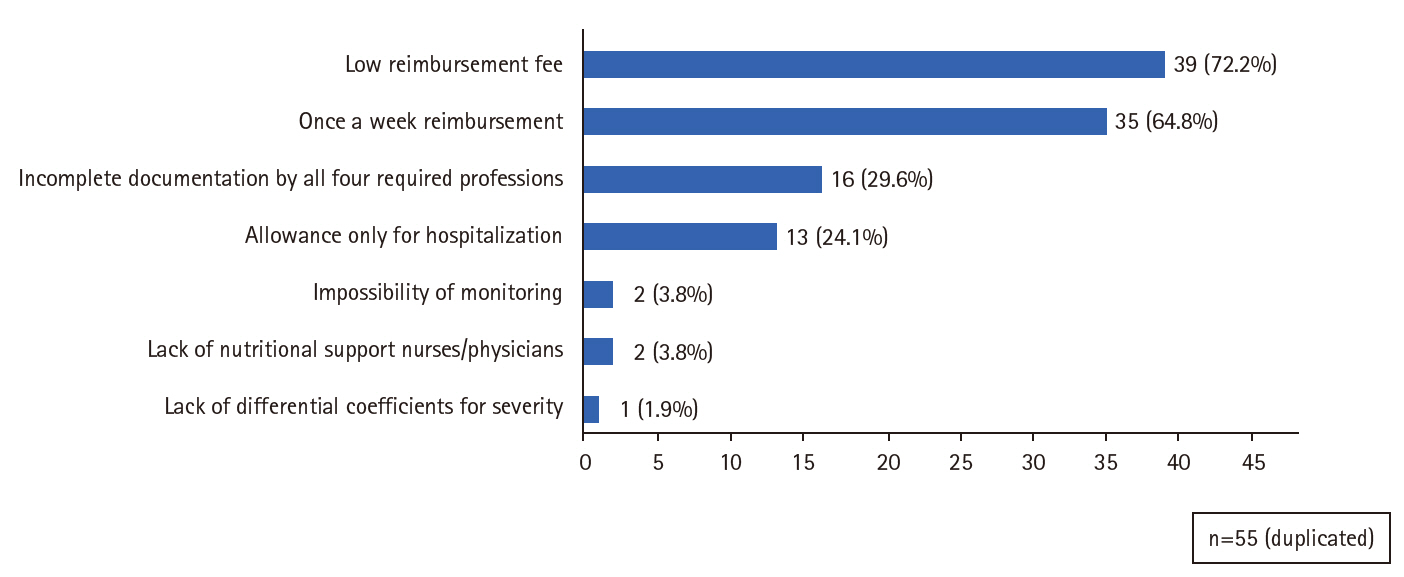
Fig. 1). The survey achieved balanced representation from physicians, clinical dietitians, and nutrition support nurses. However, the participation of pharmacists in this survey was low (
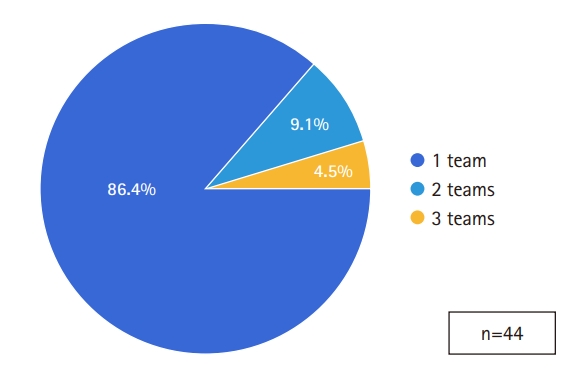
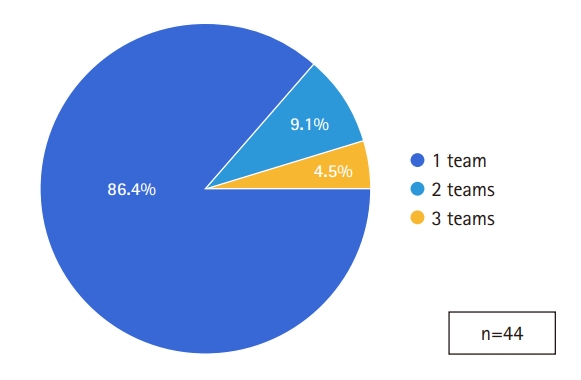
Fig. 2). Most institutions operated a single NST (n=38, 86.4%). Four institutions (9.1%) reported two teams, and two institutions operated three teams (
Fig. 3).
NST composition
Four institutions (9.1%) reported having only 1 physician in the NST. Seven institutions had 2–3 physicians, 16 had 4–7 physicians (36.3%), and 15 had 8 or more physicians (34.1%). Multidisciplinary physician participation, involving more than 3 specialties, was reported in 77.2% of institutions. For pharmacists, 16 institutions (36.3%) included 1 member, 19 had 2–3 members (43.2%), and 9 had 4 or more pharmacists (20.5%). Clinical dietitians most commonly participated in teams of 2–3 members (n=21, 47.7%), while 16 institutions had only 1 dietitian. Among nutrition support nurses, 21 institutions (47.7%) had only 1 nurse, and 14 had 2–3 nurses (31.8%). One institution reported operating without a nutrition support nurse.
The proportion of inpatients and the number of monthly consults
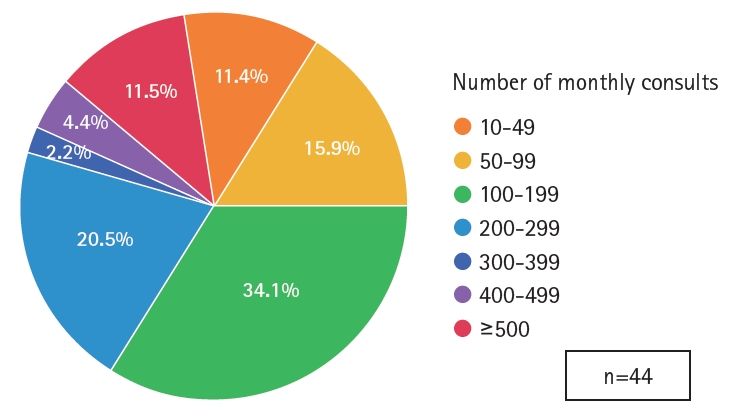
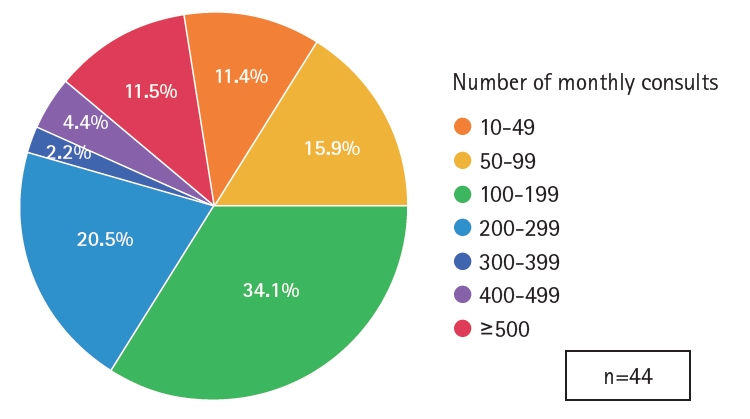
At 63% of institutions (n=34), fewer than 10% of inpatients were referred to the NST, while 19 institutions reported referral rates between 10% and 50%. We analyzed monthly consults per NSTs. Five institutions reported issuing fewer than 50 monthly consultations, while seven institutions conducted 50–99 consultations per month. Fifteen institutions issued 100–199 consults—the most common category. Nine institutions reported 200–299 consultations, one reported 300–399, and two institutions reported between 400–499 consultations per month. Five institutions reported more than 500 consults monthly (
Fig. 4).
Dedicated office space
Only 40.9% of institutions reported having a dedicated space for NST activities, while 59.1% did not.
Incentives for NSTs
Only eight institutions (18.1%) indicated the presence of formal incentives for NST activities. Official funding primarily supported departmental operating and educational expenses. In some cases, partial salary incentives were available exclusively for physicians.
NST inpatient rounding and educational activity
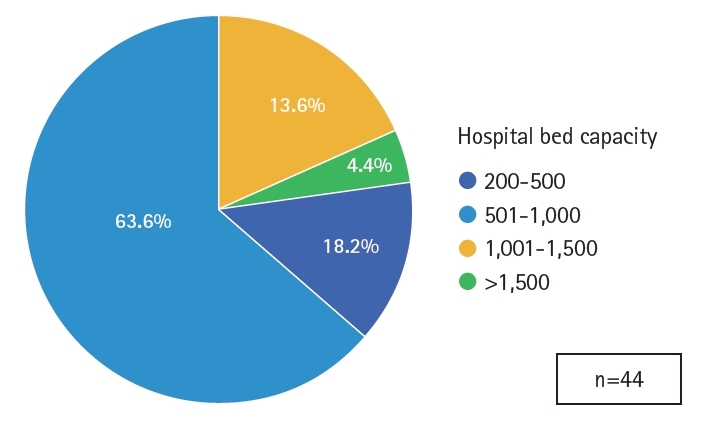
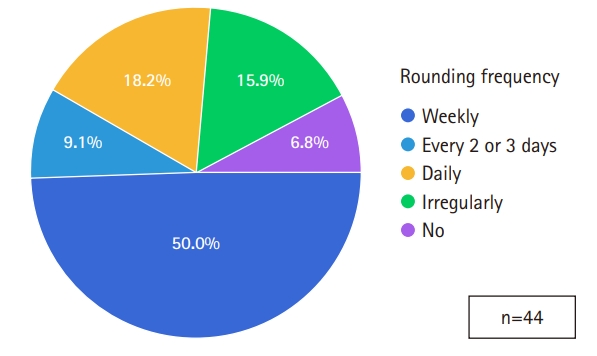
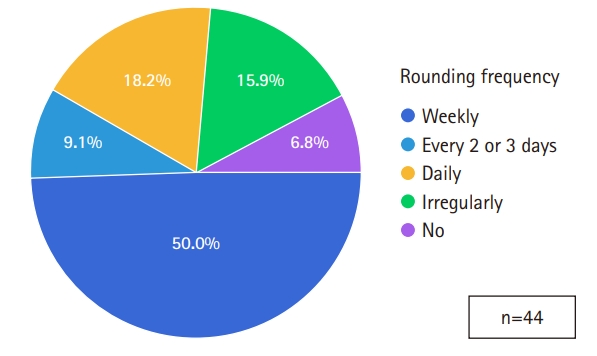
Inpatient rounding was conducted at 90.1% of institutions (
Fig. 5). Weekly rounding was most common (50%), whereas daily rounding occurred in eight institutions (18.1%). Educational programs targeting in-hospital medical staff were present at only 29.5% of institutions. Regular academic meetings, held in addition to routine rounds, were conducted at 47.7% of institutions to enhance NST capabilities.
The majority of respondents (92.6%) reported using nutritional screening tools. Of these, 70.4% used hospital-specific programs, 25.5% used the NRS-2002, and one institution reported utilizing the Global Leadership Initiative on Malnutrition criteria.
Rates of adoption of NST recommendations and associated barriers
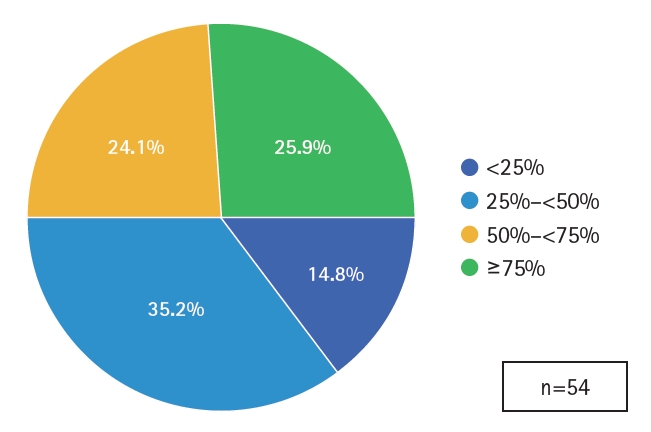
According to the survey, eight respondents indicated that fewer than 25% of NST recommendations were reflected in actual prescriptions. Nineteen respondents reported an adoption rate of 25% to <50%, while 13 indicated 50% to <75%, and 14 noted implementation rates exceeding 75% (
Fig. 6). Open-ended responses were collected to investigate the reasons for low adherence. Among those with implementation rates below 50%, the most commonly cited barriers included lack of interest from attending physicians in NST activities or patients' nutritional status, failure to review NST recommendations, department-specific clinical policies, and changes in the patient's medical condition.
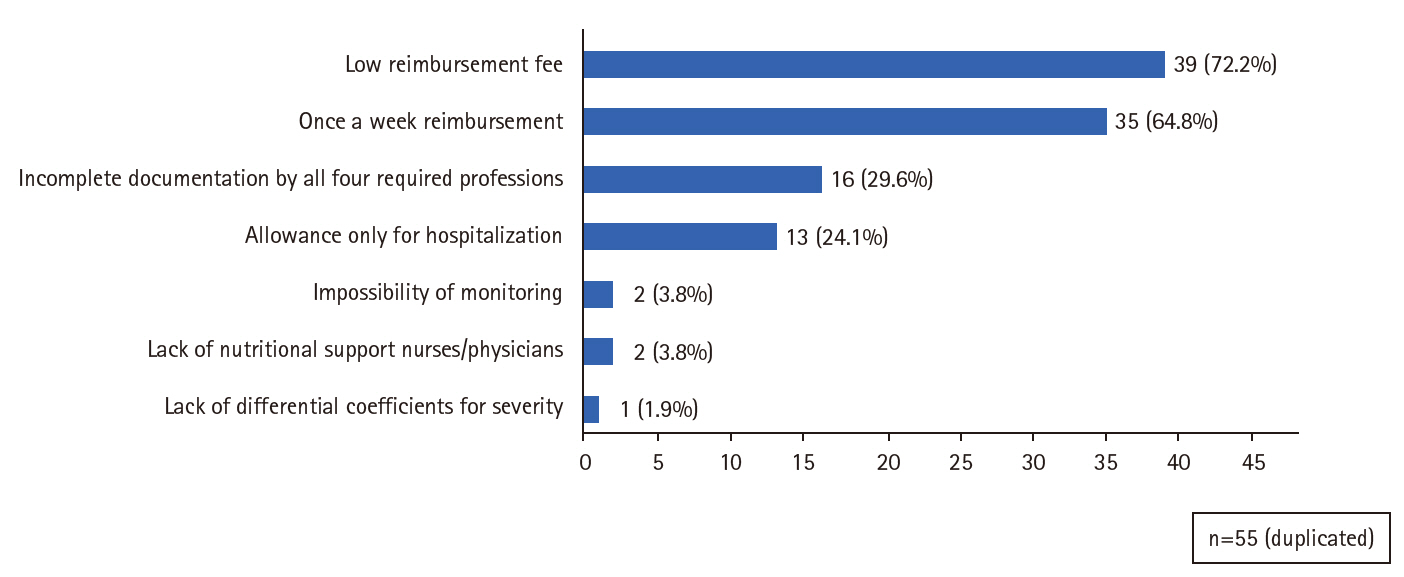
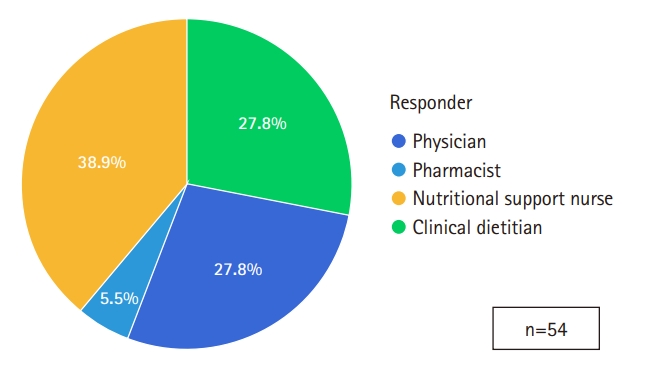
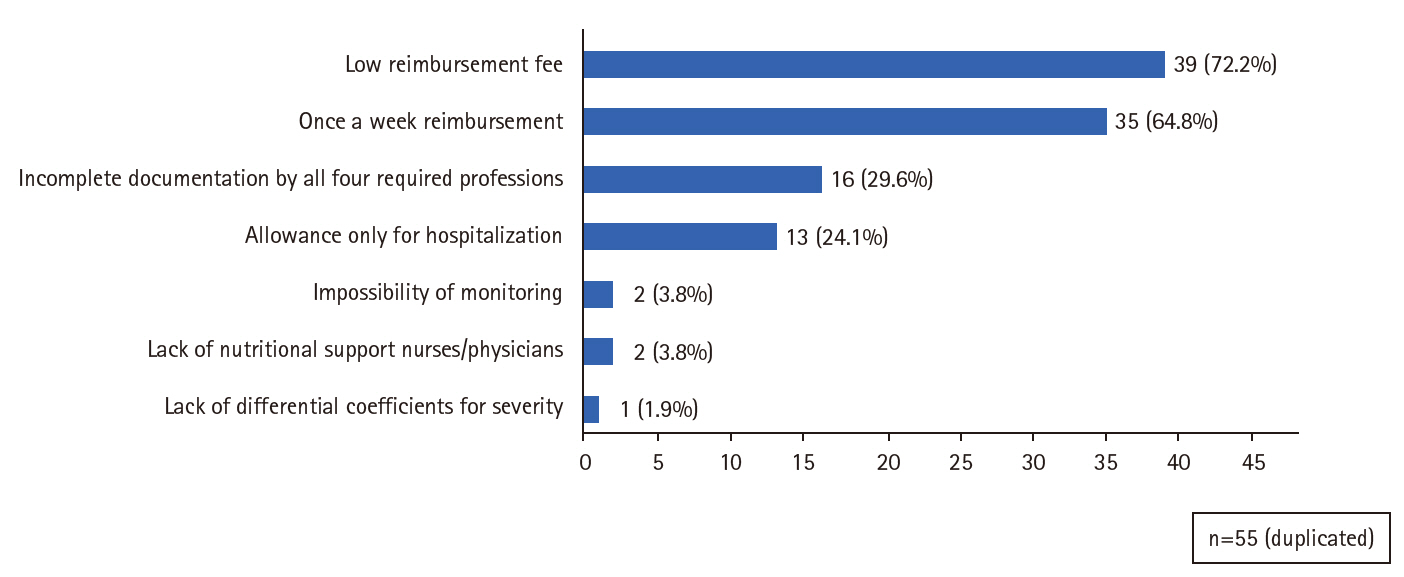
Difficulties with health insurance claims were reported by 27.2% of respondents. The reasons for reimbursement deductions included incomplete documentation by all four required professions, the absence of a pharmacist, and the lack of a pediatrician. Additional issues involved duplicate claims filed within a week, as well as situations in which patients died or were discharged after the initial response but before monitoring could be completed. Some respondents argued that the initial response, during which all four professional groups conducted nutritional assessment and prescription, should be recognized for its value. They also asserted that limiting multidisciplinary consultations to once a week is unreasonable, especially when patients require more frequent re-evaluations. These views were echoed in responses addressing the limitations of the current reimbursement system (
Fig. 7).
The most common initiatives aimed at increasing NST activation were the development of computerized prescription systems and the introduction of automated referral processes through workflow optimization. Additional institutional efforts included in-hospital education for healthcare professionals, quality improvement activities, distribution of informational materials, and promotion of NST efforts via regular multidisciplinary rounds. Proposals submitted to the Society’s programs included sharing successful NST activation cases, establishing incentive and reward systems, exchanging clinical experiences with complex cases, fostering interdisciplinary networking, clarifying team members’ roles and leadership responsibilities, and publishing comprehensive guidelines for pediatric, neonatal, and adult NST practice.
Discussion
Key results
Fifty-four responses from forty-four institutions across Korea showed that most NSTs operated in 501–1,000-bed hospitals (63.6%) and maintained single teams (86.4%), with multidisciplinary physicians in 77.2% of cases. Pharmacists, dietitians, and nurses varied in team size. Most institutions referred under 10% of inpatients, issuing predominantly 100 to 199 monthly consults. Only 40.9% had dedicated NST spaces, and 18.1% received formal incentives. Nutritional screening tools were used by 92.6%, and adoption of recommendations exceeded 75% in 25.4%.
Interpretation/comparison with previous studies
This nationwide survey conducted in 2025 provides an updated overview of hospital-based NST practices in Korea. The results underscore both the continued institutionalization of NSTs and the persistent challenges in their implementation and sustainability.
Compared with previous national surveys from 2012 and 2016, several notable trends are observed [
3-
7]. The number of hospitals with NSTs increased substantially following the introduction of reimbursement in 2014; however, this growth has plateaued in recent years. Despite improvements in infrastructure and clinical recognition, only 40.9% of institutions reported having a dedicated office for NST activities, and formal incentive systems were reported by just 18.1% of institutions.
Although NST inpatient rounding appears to be conducted consistently and effectively, educational activities for medical staff within hospitals have declined. In 2016, more than 80% of institutions reported regular academic NST meetings; in contrast, only 47.7% indicated such activities in 2025 [
5]. However, the adoption of validated nutritional screening tools has gradually increased. Notably, use of the NRS-2002 rose from 7.2% in 2016 to 25.5% in 2025, indicating a shift toward more standardized assessment practices [
5]
Adherence to NST recommendations remains suboptimal. Although the proportion of institutions reporting implementation rates below 25% decreased from 34.3% in 2016 to 14.8% in 2025, nearly half of the institutions still reported adherence rates of less than 50%. Multiple factors, including insufficient physician awareness, individualized clinical treatment policies, and fluctuating patient conditions, contribute to the challenges of effectively implementing NST recommendations. While such recommendations may sometimes conflict with the attending physician’s diagnostic and prescribing authority, comprehensive patient evaluation and evidence-based nutritional support are essential. Previous studies have shown that in-hospital educational initiatives for medical residents can significantly improve awareness, referral rates, and compliance, underscoring the importance of institutional support and visibility [
8]. Despite ongoing challenges, it is crucial to reinforce educational and promotional activities within hospitals to improve adherence to NST recommendations.
Systemic and operational barriers continue to hinder the effectiveness of NST. These include limited human resources, high workloads among clinical dietitians and nurses, pharmacist shortages, and stringent reimbursement criteria requiring documentation from all four professional roles. The current reimbursement system does not account for case complexity or patient severity, which may compromise care quality by prioritizing quantity over quality [
7]. Furthermore, professional burnout has become a growing concern, particularly in settings without sufficient incentive systems or dedicated nurse staffing workspaces.
Despite these limitations, a growing body of evidence supports the clinical benefits of NST implementation. Several large-scale studies from Korea have demonstrated significant reductions in mortality among critically ill patients—including those with sepsis, acute respiratory distress syndrome, and COVID-19—following NST consultation according to the American Society for Parenteral and Enteral Nutrition/ European Society for Clinical Nutrition and Metabolism guideline. Notably, early NST intervention can improve patients’ overall nutritional status. While some studies have not demonstrated survival benefits despite improved nutritional delivery, the association between multidisciplinary support and enhanced nutritional adequacy remains consistent [
9-
15]
To advance NST functionality, nutrition support nurses emphasized the importance of reeducation and advanced training programs for themselves [
16]. The survey also revealed substantial demand for peer-to-peer knowledge exchange, comprehensive clinical guidelines, and targeted educational resources to address complex case management. These findings suggest that KSSMN should take a more proactive role in promoting quality improvement.
This study has several limitations. The participating institutions may represent hospitals with relatively well-established NSTs, introducing potential selection bias. Additionally, the survey relied on self-reported responses without statistical testing, which limits its generalizability and inferential analysis.
Conclusion
While NST activity in Korea has expanded over the past decade, significant challenges remain in operational sustainability, clinical adoption, and workforce support. Addressing these issues through targeted education, policy reform, and multidisciplinary engagement is essential to ensure the long-term effectiveness of NSTs in hospital-based nutritional care.
Authors’ contribution
All work was done by So Hyun Nam.
Conflict of interest
So Hyun Nam has served as the editor of the Annals of Clinical Nutrition and Metabolism since 2022. However, she was not involved in the peer review process or decision-making regarding publication. Otherwise, no potential conflict of interest relevant to this article was reported.
Funding
None.
Data availability
Contact the corresponding author for research data availability.
Acknowledgments
We would like to express our deepest gratitude to all members of the nutrition support team (NST) who generously contributed their time and insights to participate in this survey.
Supplementary materials
Correction
This article was corrected on November 13, 2025, to revise the article type.
Fig. 1.Distribution of hospital bed capacity.
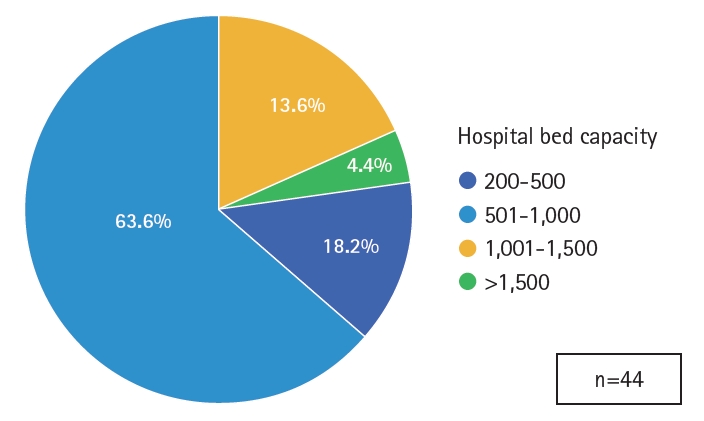
Fig. 2.Distribution of responders’ roles in nutrition support teams.
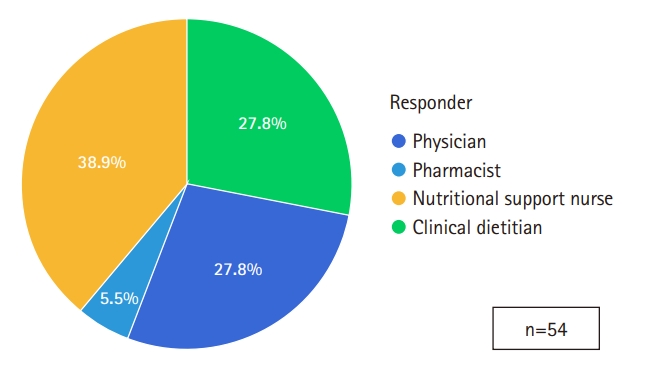
Fig. 3.Number of nutrition support teams per hospital.
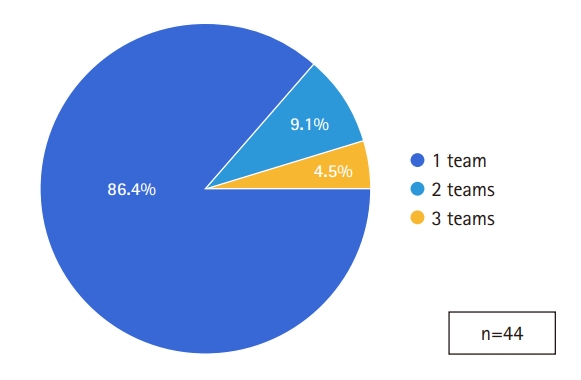
Fig. 4.The number of monthly consults per nutrition support team.
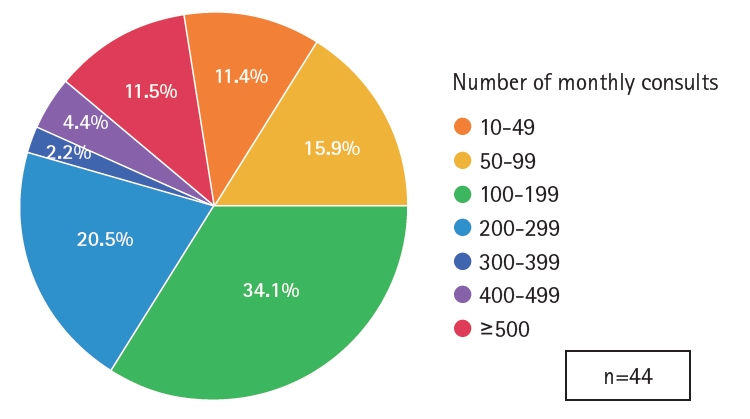
Fig. 5.Frequency of nutrition support team inpatient rounding.
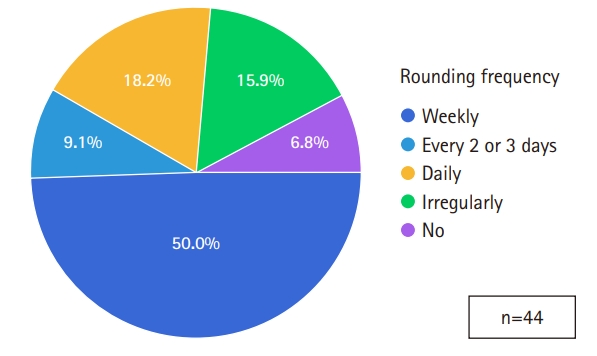
Fig. 6.Rates of adoption of nutrition support team recommendations.
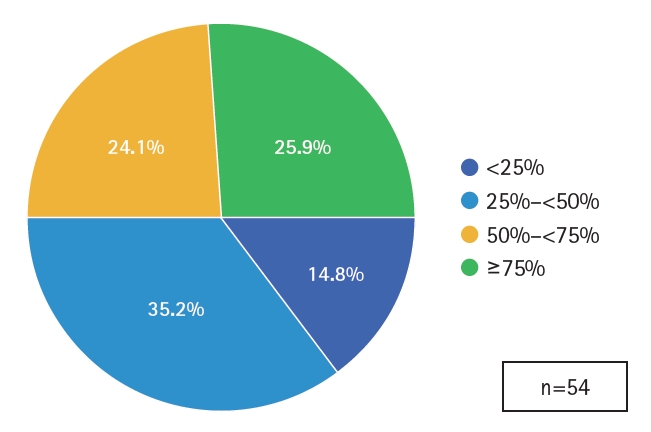
Fig. 7.The responses addressing the shortcomings of the reimbursement system.
References
- 1. Lee YM, Kim SH, Kim YS, Kim EM, Kim JY, Keum MA, et al. Nutritional status of Korean hospitalized patients: a multi-center preliminary survey. J Clin Nutr 2014;6:71-8. Article
- 2. Vandenbroucke JP, von Elm E, Altman DG, Gotzsche PC, Mulrow CD, Pocock SJ, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration-a Korean translation. Ewha Med J 2024;47:e31.ArticlePubMedPMCPDF
- 3. Seo KW, Kang GH, Kong SH, Ryu SW, Park JS, Park JW, et al. Current status of nutritional supports on surgical Patients in Korea: a nationwide survey. Surg Metab Nutr 2012;3:45-52.
- 4. Cho JY, Kim JT, Kim SL. Survey on the state of nutrition support team (NST) activity: comparison of the questionnaire survey 2016 vs. 2005 and the state of NST activity since the Introduction of the medical insurance fee. J Clin Nutr 2016;8:38-44. Article
- 5. Sul JY, Kim JG. The present and future of nutrition support team. Surg Metab Nutr 2019;10:1-4. Article
- 6. Cheon S, Oh SH, Kim JT, Choi HG, Park H, Chung JE. Nutrition therapy by nutrition support team: a comparison of multi-chamber bag and customized parenteral nutrition in hospitalized patients. Nutrients 2023;15:2531.ArticlePubMedPMC
- 7. Shin D. Reimbursement of nutritional support team, what is the problem and how can we manage it? J Clin Nutr 2015;7:2-8. Article
- 8. Kim KJ, Choe I, Moon KR. Nutritional support team through the consciousness questionnaire to residents. J Kor Soc Health-Syst Pharm 2013;30:512-22. Article
- 9. Oh TK, Lee K, Cho J, Song IA. Multidisciplinary nutritional support team and mortality in critically ill patients with acute respiratory distress syndrome. Acta Anaesthesiol Scand 2024;68:1487-93. ArticlePubMed
- 10. Song IA, Lee K, Lee S, Kim K, Oh TK. Implementation of a multidisciplinary nutritional support team and clinical outcomes in critically ill patients with COVID-19. Clin Nutr 2024;43:315-21. ArticlePubMed
- 11. Lee K, Song IA, Lee S, Kim K, Oh TK. Multidisciplinary nutritional support team and survival outcomes in patients with sepsis: a nationwide population-based cohort study in South Korea. Eur J Clin Nutr 2024;78:765-71. ArticlePubMedPDF
- 12. Lee NG, Kim HJ, Kang JG, Jeon DH, Kwak MS, Nam SH. Effects of nutritional status and support on the survival of COVID-19 patients in a single tertiary-center intensive care unit in Korea: a case-control study. Ann Clin Nutr Metab 2023;15:30-7. Article
- 13. Cho J, Park YS, Park DJ, Kim S, Lee H, Kim M, et al. Bridging policy and service performance of hospital-based nutrition support by healthcare information technology. Nutrients 2021;13:595.ArticlePubMedPMC
- 14. Seol EM, Suh YS, Ju DL, Bae HJ, Kim E, Lee HJ. Nutrition support team reconsultation during nutrition therapy in Korea. J Parenter Enteral Nutr 2021;45:357-65. ArticlePDF
- 15. Kim SH, Bu SY. Effect of the timing of nutritional support team intervention on nutritional status on patients receiving enteral nutrition. Clin Nutr Res 2021;10:1-13. ArticlePubMedPMCPDF
- 16. Park JY, Song JM, Min JK. Nutrition support nurse: roles and tasks. J Clin Nutr 2020;12:2-6. Article




 E-submission
E-submission KSPEN
KSPEN KSSMN
KSSMN ASSMN
ASSMN JSSMN
JSSMN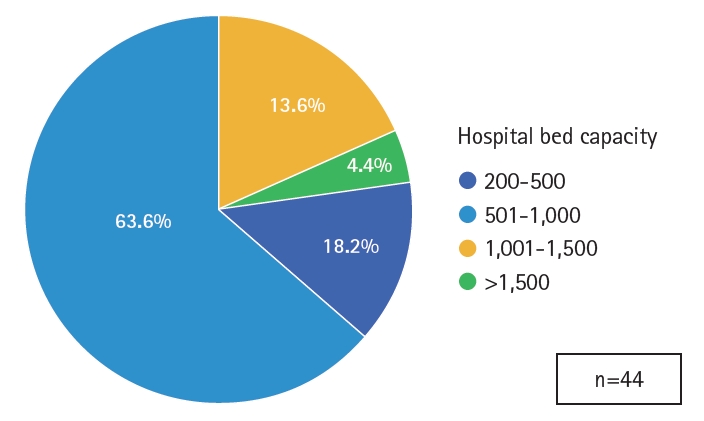
 Cite
Cite

