-
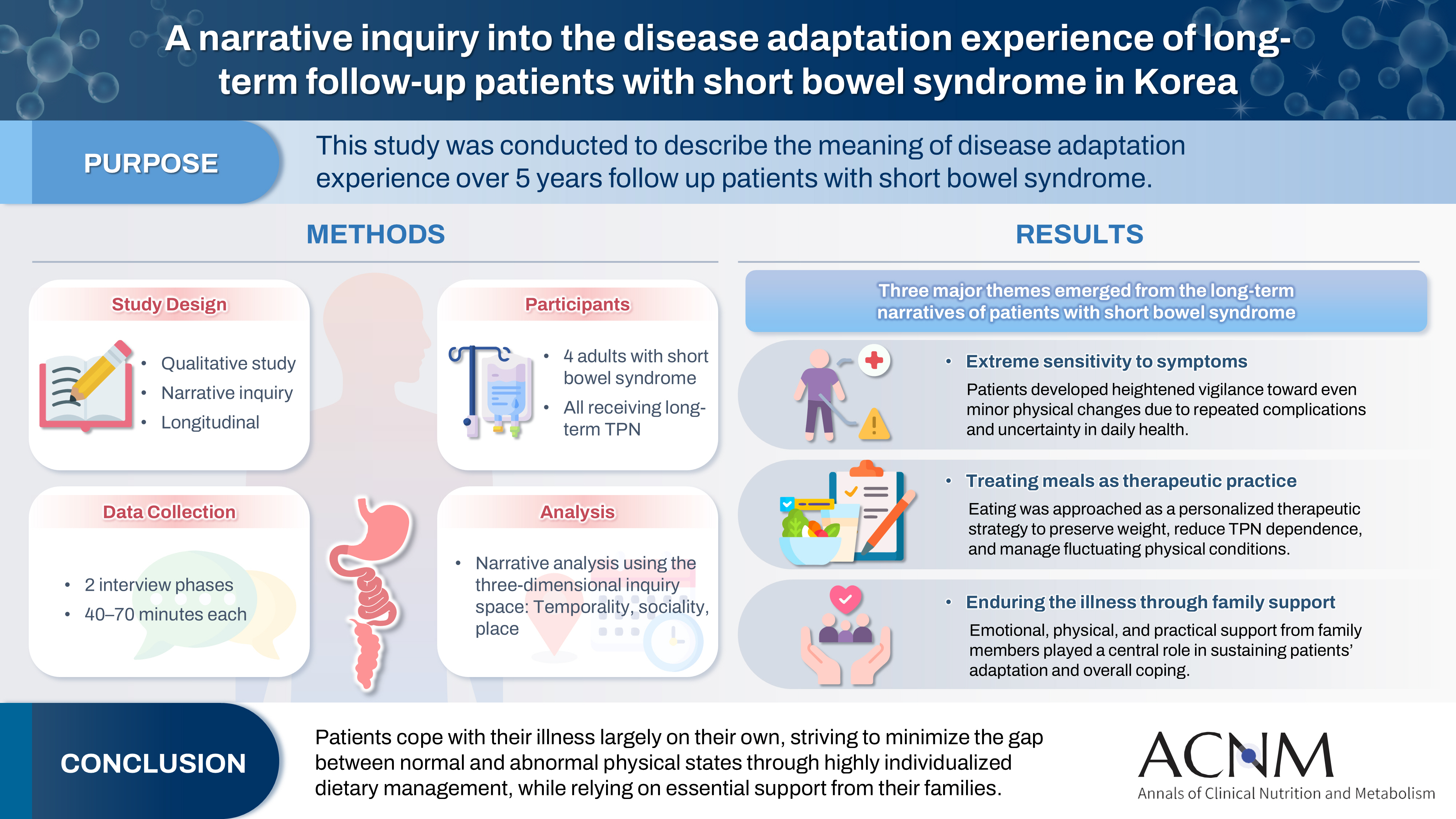
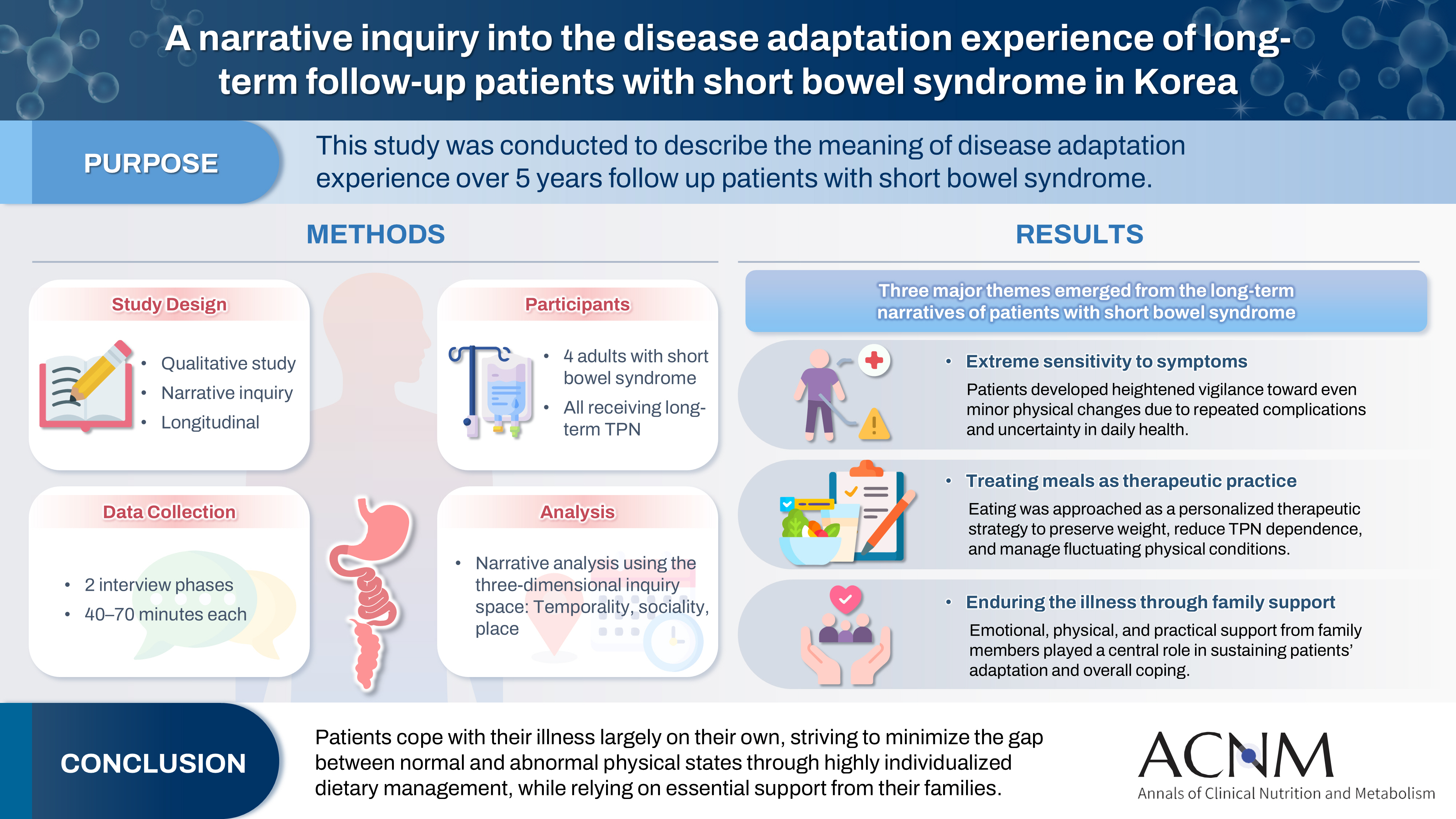
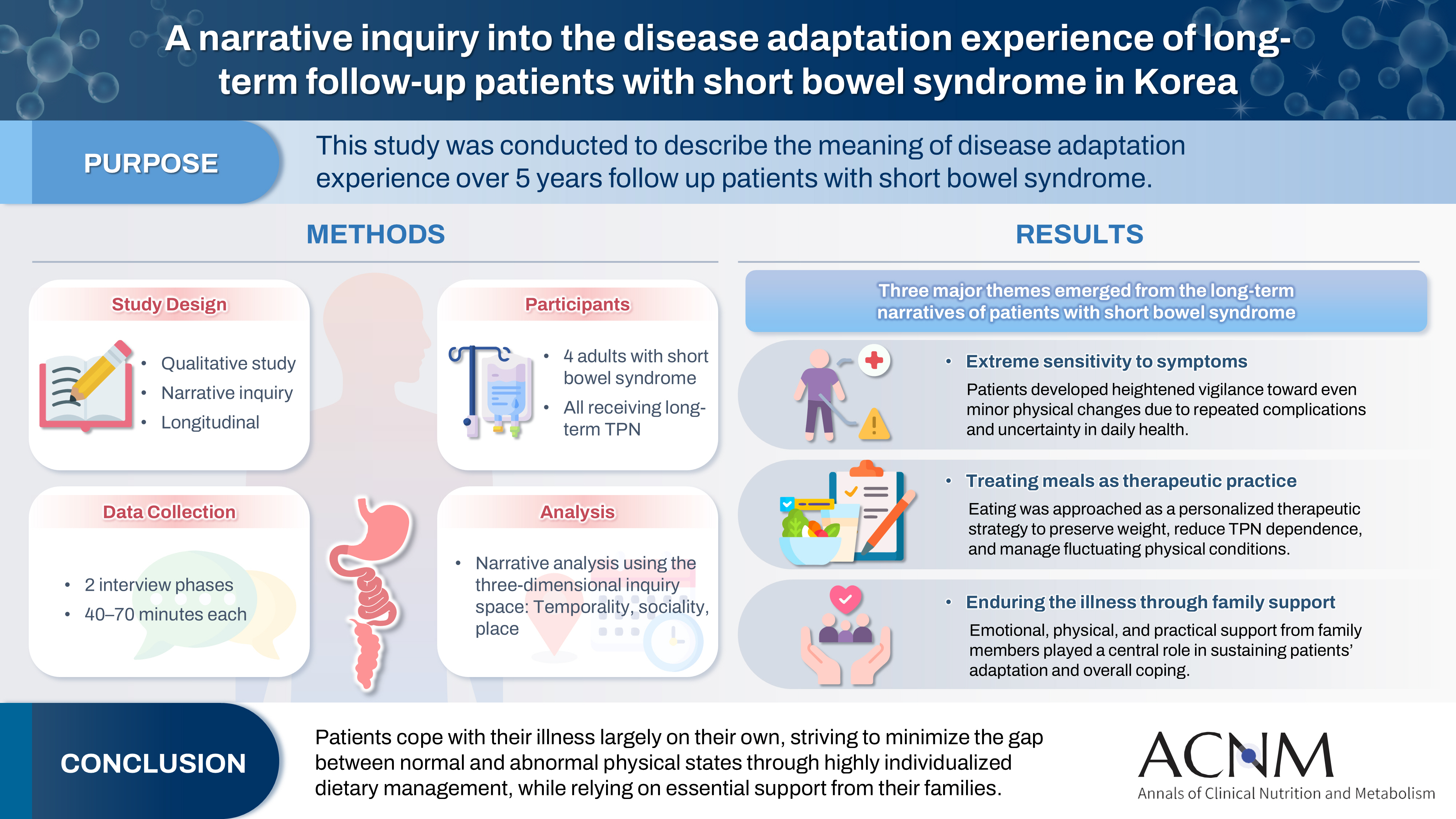
A narrative inquiry into the disease adaptation experience of long-term follow-up patients with short bowel syndrome in Korea
-
Eun-Mi Seol, Eunjung Kim
-
Ann Clin Nutr Metab 2025;17(3):188-195. Published online December 1, 2025
-
DOI: https://doi.org/10.15747/ACNM.25.0028
-
-
 Graphical Abstract Graphical Abstract
 Abstract Abstract
 PDF PDF Supplementary Material Supplementary Material
 - Purpose
This study was conducted to describe the meaning of disease adaptation experience over a 5-year long-term follow-up of patients with short bowel syndrome.
Methods
Four patients were recruited from a tertiary hospital in Korea. This study was conducted through first and second interviews from January 2019 to July 2022. The transcribed data were analyzed using narrative methods.
Results
The mean age of the participants was 64 years, and the mean treatment period after small bowel resection was 100 months. The participants lost a mean of 19.3 kg body weight and all were receiving home total parenteral nutrition 2–7 days a week. The meaning of the experience of adapting to the disease for patients was found to be “extremely sensitive to the symptoms,” “considering eating food as another effective treatment method,” and “enduring the disease through family affection.”
Conclusion
Patients are struggling alone to cope with physical symptoms and adapt to their disease. For this, they are doing their best to narrow the gap between normal and abnormal physical conditions by thoroughly implementing diet therapy according to their physical characteristics. This entire process is supported by their families.
-
A practical guide for enteral nutrition from the Korean Society for Parenteral and Enteral Nutrition: Part II. selection and initiation of enteral feeding routes
-
Ja Kyung Min, Ye Rim Chang, Bo-Eun Kim, In Seok Lee, Jung Mi Song, Hyunjung Kim, Jae Hak Kim, Kyung Won Seo, Sung Shin Kim, Chi-Min Park, Jeongyun Park, Eunjung Kim, Eunmi Sul, Sung-Sik Han, Jeong Wook Kim, Seungwan Ryu, Minji Seok, Jinhee Yoon, Eunhee Kong, Youn Soo Cho, Jeong Meen Seo, for KSPEN Enteral Nutrition Committee
-
Ann Clin Nutr Metab 2025;17(3):165-171. Published online December 1, 2025
-
DOI: https://doi.org/10.15747/ACNM.25.0037
-
-
 Abstract Abstract
 PDF PDF
- Purpose
We developed evidence-based recommendations for selecting and initiating the enteral nutrition (EN) delivery route in adult and pediatric patients to improve safety and standardize practice in Korea.
Methods
Key questions covered feeding tube selection, methods to verify tube placement, confirmation in pediatric patients, and timing of EN following percutaneous endoscopic gastrostomy (PEG). Recommendations were drafted and refined through multidisciplinary expert consensus under the Korean Society for Parenteral and Enteral Nutrition (KSPEN).
Results
Feeding tube selection should be based on gastrointestinal anatomy, function, and expected EN duration. Short-term feeding is recommended with nasogastric or orogastric tubes, whereas long-term feeding should use percutaneous or surgical routes such as PEG. Tube position must always be verified before use, preferably with radiography or pH testing; auscultation alone is unreliable and should not be used. In pediatric patients, radiographic confirmation remains the gold standard, although pH testing and insertion-length assessment may be considered when imaging is not feasible. After PEG, EN can be initiated safely within 4 hours in both adults and children without increasing complications if trained staff monitor for leakage or infection.
Conclusion
This guideline offers a structured framework for safe and timely EN tailored to patient characteristics. Early verification and multidisciplinary collaboration help reduce complication, improving outcomes of EN therapy.
-
A practical guide for enteral nutrition from the Korean Society for Parenteral and Enteral Nutrition: Part I. prescribing enteral nutrition orders
-
Ye Rim Chang, Bo-Eun Kim, In Seok Lee, Youn Soo Cho, Sung-Sik Han, Eunjung Kim, Hyunjung Kim, Jae Hak Kim, Jeong Wook Kim, Sung Shin Kim, Eunhee Kong, Ja Kyung Min, Chi-Min Park, Jeongyun Park, Seungwan Ryu, Kyung Won Seo, Jung Mi Song, Minji Seok, Eun-Mi Seol, Jinhee Yoon, Jeong Meen Seo, for KSPEN Enteral Nutrition Committee
-
Ann Clin Nutr Metab 2025;17(1):3-8. Published online April 1, 2025
-
DOI: https://doi.org/10.15747/ACNM.25.0002
-
-
 Abstract Abstract
 PDF PDF
- Purpose
This study aimed to develop a comprehensive practical guide for enteral nutrition (EN) designed to enhance patient safety and reduce complications in Korea. Under the leadership of the Korean Society for Parenteral and Enteral Nutrition (KSPEN), the initiative sought to standardize EN procedures, improve decision-making, and promote effective multidisciplinary communication.
Methods
The KSPEN EN committee identified key questions related to EN practices and organized them into seven sections such as prescribing, delivery route selection, formula preparation, administration, and quality management. Twenty-one experts, selected based on their expertise, conducted a thorough literature review to formulate evidence-based recommendations. Drafts underwent peer review both within and across disciplines, with final revisions completed by the KSPEN Guideline Committee. The guide, which will be published in three installments, addresses critical elements of EN therapy and safety protocols.
Results
The practical guide recommends that EN orders include detailed elements and advocates the use of electronic medical records for communication. Standardized prescription forms and supplementary safety measures are outlined. Review frequency is adjusted according to patient condition—daily for critically ill or unstable patients and as dictated by institutional protocols for stable patients. Evidence indicates that adherence to these protocols reduces mortality, complications, and prescription errors.
Conclusion
The KSPEN practical guide offers a robust framework for the safe delivery of EN tailored to Korea’s healthcare context. It emphasizes standardized protocols and interdisciplinary collaboration to improve nutritional outcomes, patient safety, and operational efficiency. Rigorous implementation and monitoring of adherence are critical for its success.
-
Citations
Citations to this article as recorded by  - Bridging evidence and clinical practice: a practical guide for enteral nutrition from the Korean Society for Parenteral and Enteral Nutrition
Suk-Kyung Hong
Ann Clin Nutr Metab.2025; 17(1): 1. CrossRef
-
6,881
View
-
183
Download
-
1
Crossref
-
Long-Term Changes of Body Mass Index and Nutritional Biochemical Markers in the Obese Elderly with Gastric Cancer
-
Eunjung Kim, Ji-Hyeon Park, Eun-Mi Seol, Seong-Ho Kong, Do Joong Park, Han-Kwang Yang, Hyuk-Joon Lee
-
Ann Clin Nutr Metab 2021;13(2):52-61. Published online December 31, 2021
-
DOI: https://doi.org/10.15747/ACNM.2021.13.2.52
-
-
 PDF PDF
-
In-line Filtration in Parenteral Nutrition
-
Eunjung Kim, Eun-Mi Seol
-
J Clin Nutr 2019;11(1):1-4. Published online June 30, 2019
-
DOI: https://doi.org/10.15747/jcn.2019.11.1.1
-
-
 Abstract Abstract
 PDF PDF
Metabolic abnormalities and catheter-related infections are common complications of parenteral nutrition (PN). Particulate contamination is a catheter-related complication can occur when administering PN: mixing the electrolytes, trace elements, vitamins into the PN, or puncturing a rubber stopper at the PN formulation. In addition, the aggregation of the components of the PN solution by a drug incompatibility reaction could be related to particulate contamination. PN contaminated with precipitates, insoluble particles, and bacteria was reported as the cause of the death of a patient. The Food and Drug Administration recommended that the filters be used during PN administration. In-line filters can retain the bacteria and insoluble particles in PN solutions, and prevent their infusion into the patient. Therefore, in-line filters are recommended to prevent catheter-related complications that can occur during PN infusion. A 0.2µ filter for lipid-free PN and a 1.2µ filter for lipid-containing PN solutions can be used. On the other hand, when a filter is applied, the infusion rate can decrease and the economic burden will increase for patients requiring long-term PN. In addition, small particles, such as viruses, polymers, and proteins cannot be filtered out completely. In conclusion, in-line filers are recommended to prevent catheter-related complications that can occur during PN administration, but there are no international standardized guidelines. Therefore, standardized guidelines will be needed based on evidence accompanied by clinical trials. In addition, in-line filter applications should be considered in the clinical field depending on the patient’s condition.
-
Recovery Pattern of the Nutritional Status after Surgical Treatment for Pancreatic Head Disease: Compared with Malignancy and Non-malignancy
-
Eunjung Kim, Youngmin Han, Hongbeom Kim, Wooil Kwon, Sun-Whe Kim, Jin-Young Jang
-
Surg Metab Nutr 2018;9(2):51-58. Published online December 30, 2018
-
DOI: https://doi.org/10.18858/smn.2018.9.2.51
-
-
 Abstract Abstract
 PDF PDF
-
Purpose: Malnutrition affects the clinical outcomes of pancreatic disease. On the other hand, the changes in the nutritional status stratified by malignant and non-malignant diseases after surgery still need to be determined. The aim was to confirm the changing nutritional status and clinical outcomes after a pancreatoduodenectomy according to malignant and non-malignant disease. Materials and Methods: Data were collected prospectively from 157 patients between 2009 and 2015. The nutritional status was classified as well-nourished, at-risk of malnutrition, and malnourished by a Mini Nutrition Assessment. The clinical outcomes were assessed using the postoperative complication, hospital stay, biochemical nutritional markers, and quality-of-life (QOL). Results: Preoperatively, the proportion of malnourished status in the malignant disease group (group B) were 66.7% and 33.3% in the non-malignancy group (group A). The malnutrition rate in group B was higher than that in group A at 3, 6, and 12 months after surgery (58.1% vs. 41.9%, 90.0% vs. 10.0, 77.8% vs. 22.2%, respectively). The preoperative QOL was significantly lower in group B than in group A (P<.001); however, the QOL was comparable between the two groups after surgery. The body mass index was unrecovered after surgery in all groups. Conclusion: Patients with malignant pancreatic disease are more likely to suffer from a poor nutritional status than those with non-malignant pancreatic disease. One year after the pancreatoduodenctomy, the at-risk of malnutrition and malnourished rate were found to be over 70% in all patients. Therefore, more efforts will be needed to improve the nutritional status in pancreatic head disease.
-
Citations
Citations to this article as recorded by  - Factors Affecting Nutritional Index and Length of Stay in Pancreatic Cancer in the Older Adults
So Young Jun, Mo Na Choi, Joon Seong Park, Hyang Kyu Lee
Asian Oncology Nursing.2023; 23(3): 91. CrossRef
-
914
View
-
3
Download
-
1
Crossref
|