Indexed in:
Scopus, KCI, KoreaMed
Scopus, KCI, KoreaMed

Search
- Page Path
- HOME > Search
Guideline
- A practical guide for enteral nutrition from the Korean Society for Parenteral and Enteral Nutrition: Part II. selection and initiation of enteral feeding routes
- Ja Kyung Min, Ye Rim Chang, Bo-Eun Kim, In Seok Lee, Jung Mi Song, Hyunjung Kim, Jae Hak Kim, Kyung Won Seo, Sung Shin Kim, Chi-Min Park, Jeongyun Park, Eunjung Kim, Eunmi Sul, Sung-Sik Han, Jeong Wook Kim, Seungwan Ryu, Minji Seok, Jinhee Yoon, Eunhee Kong, Youn Soo Cho, Jeong Meen Seo, for KSPEN Enteral Nutrition Committee
- Ann Clin Nutr Metab 2025;17(3):165-171. Published online December 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0037
-
 Abstract
Abstract
 PDF
PDF - Purpose
We developed evidence-based recommendations for selecting and initiating the enteral nutrition (EN) delivery route in adult and pediatric patients to improve safety and standardize practice in Korea.
Methods
Key questions covered feeding tube selection, methods to verify tube placement, confirmation in pediatric patients, and timing of EN following percutaneous endoscopic gastrostomy (PEG). Recommendations were drafted and refined through multidisciplinary expert consensus under the Korean Society for Parenteral and Enteral Nutrition (KSPEN).
Results
Feeding tube selection should be based on gastrointestinal anatomy, function, and expected EN duration. Short-term feeding is recommended with nasogastric or orogastric tubes, whereas long-term feeding should use percutaneous or surgical routes such as PEG. Tube position must always be verified before use, preferably with radiography or pH testing; auscultation alone is unreliable and should not be used. In pediatric patients, radiographic confirmation remains the gold standard, although pH testing and insertion-length assessment may be considered when imaging is not feasible. After PEG, EN can be initiated safely within 4 hours in both adults and children without increasing complications if trained staff monitor for leakage or infection.
Conclusion
This guideline offers a structured framework for safe and timely EN tailored to patient characteristics. Early verification and multidisciplinary collaboration help reduce complication, improving outcomes of EN therapy.
- 196 View
- 7 Download

Original Article
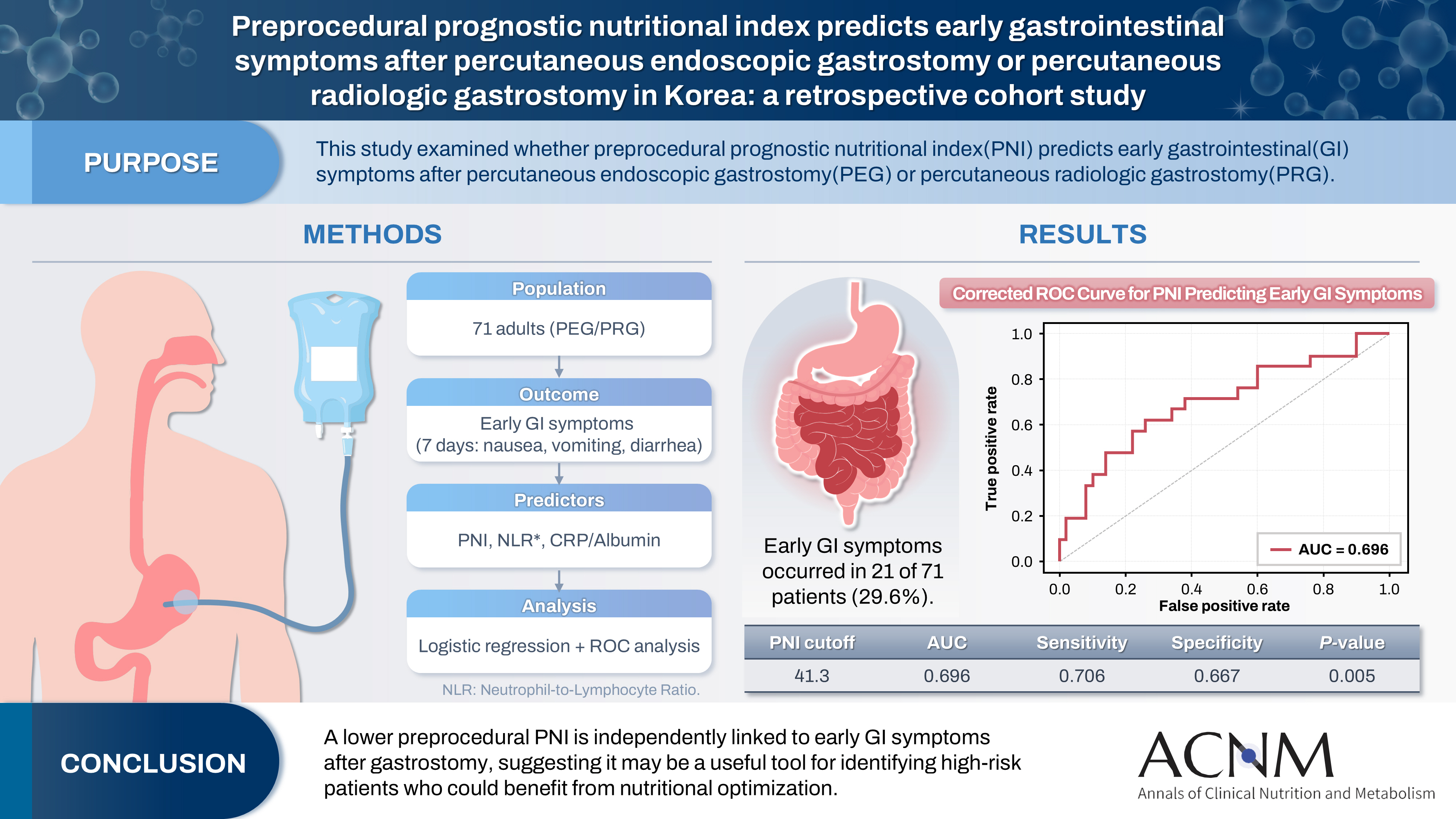
- Preprocedural prognostic nutritional index predicts early gastrointestinal symptoms after percutaneous endoscopic gastrostomy or percutaneous radiologic gastrostomy in Korea: a retrospective cohort study
- Yoonhong Kim, Jee Young Lee, Yeajin Moon, Seung Hun Lee, Kyung Won Seo, Ki Hyun Kim
- Ann Clin Nutr Metab 2025;17(3):196-202. Published online December 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0032
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 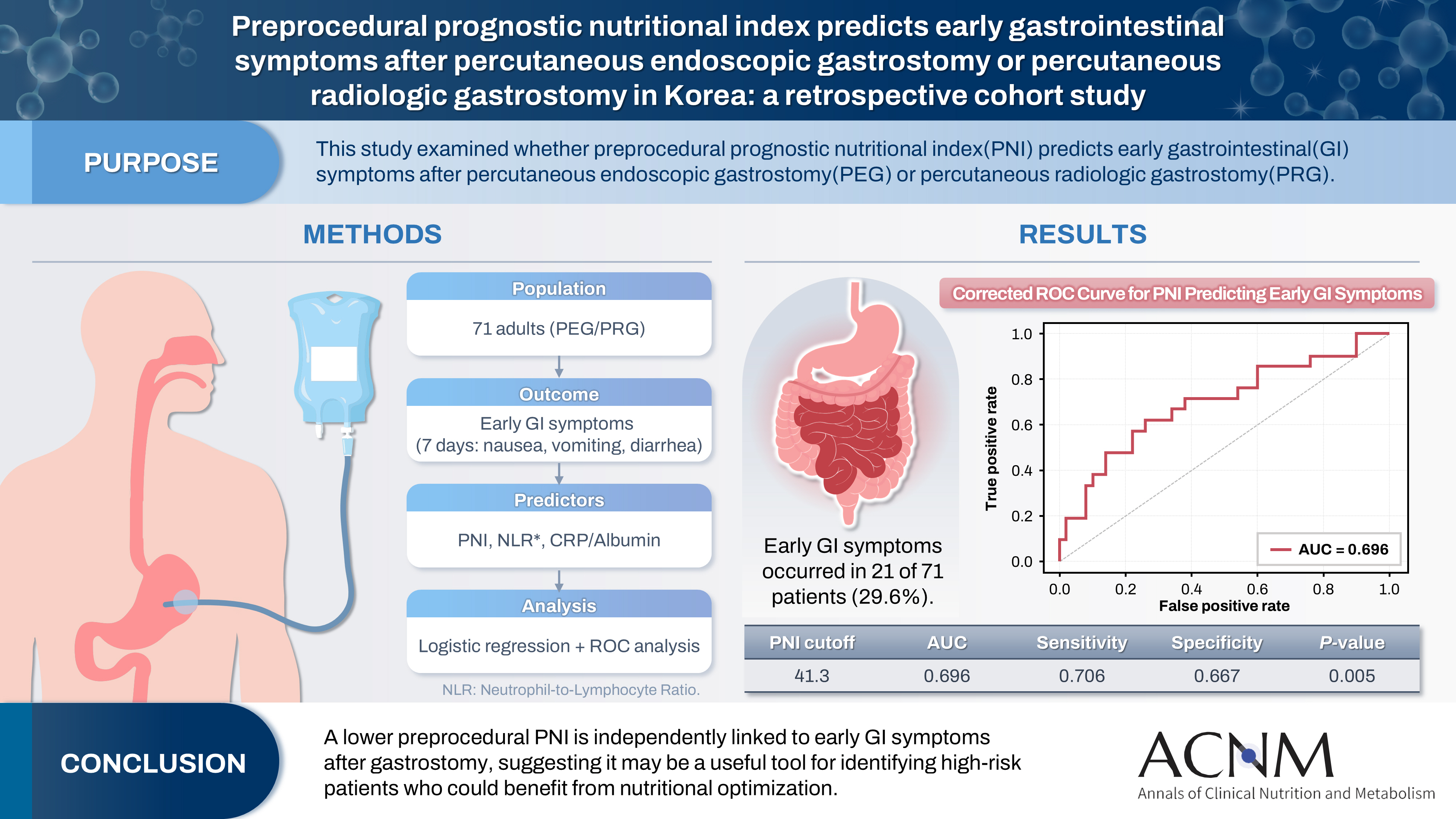
- Purpose
The prognostic nutritional index (PNI) reflects immunonutritional status and is a well-established predictor of surgical outcomes. Although its association with post-gastrostomy mortality has been documented, its relationship with early gastrointestinal (GI) symptoms remains unclear. This study aimed to evaluate whether the preprocedural PNI predicts early GI symptoms following percutaneous gastrostomy, including percutaneous endoscopic gastrostomy (PEG) and percutaneous radiologic gastrostomy (PRG).
Methods
This retrospective study included 71 adults who underwent PEG or PRG. Early GI symptoms, such as nausea, vomiting, and diarrhea, occurring within 7 days were recorded. The preprocedural PNI, neutrophil-to-lymphocyte ratio (NLR), and the C-reactive protein (CRP)-to-albumin ratio were analyzed using logistic regression to identify predictors. Receiver operating characteristic (ROC) analysis was performed to assess the PNI’s discriminative performance.
Results
Early GI symptoms occurred in 21 of 71 patients (29.6%). In univariate analysis, the PNI (P=0.009) and CRP-to-albumin ratio (P=0.018) were significant predictors, whereas NLR was not (P=0.125). After adjustment for potential confounders, including age, sex, body mass index, and NLR, the PNI remained an independent predictor of early GI symptoms (adjusted odds ratio, 0.90; 95% confidence interval, 0.83–0.98; P=0.021). ROC analysis for the PNI produced an area under the curve of 0.696, with an optimal cutoff value of 41.3 (sensitivity 70.6%, specificity 66.7%).
Conclusion
A lower preprocedural PNI is independently associated with the development of early GI symptoms after gastrostomy. The PNI may serve as a practical screening tool to identify high-risk patients who could benefit from preemptive nutritional optimization.
- 182 View
- 9 Download

Interesting image
- Penetration of a nasogastric tube by a stylet during insertion
- Akihide Takami, Haruka Tsuji, Kazuya Omura
- Ann Clin Nutr Metab 2025;17(3):210-211. Published online December 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0029
- 120 View
- 7 Download

Original Articles
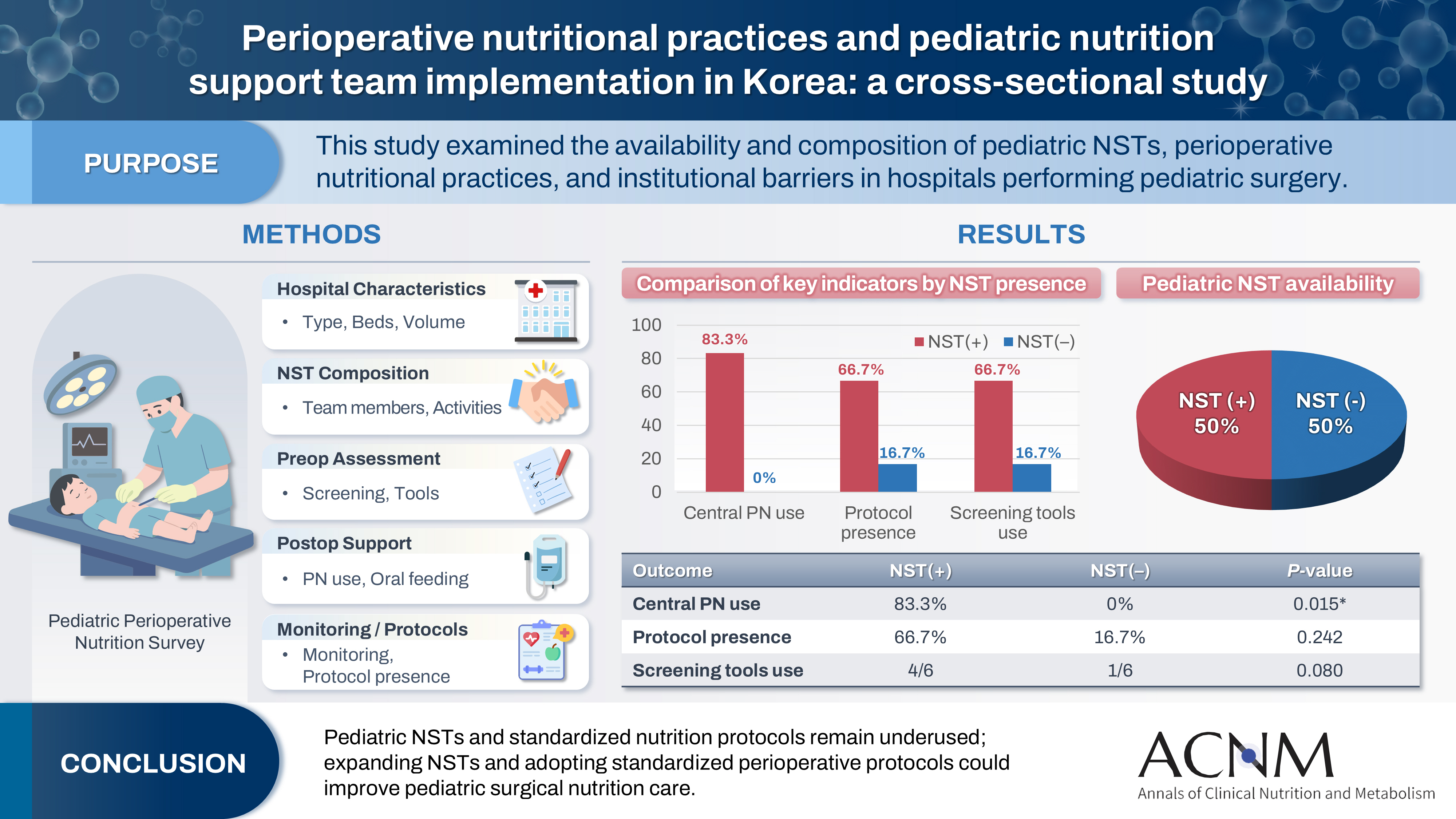
- Perioperative nutritional practices and pediatric nutrition support team implementation in Korea: a cross-sectional study
- Dayoung Ko, Honam Hwang, Hee-Beom Yang, Joong Kee Youn, Hyun-Young Kim
- Ann Clin Nutr Metab 2025;17(3):181-187. Published online December 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0027
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material 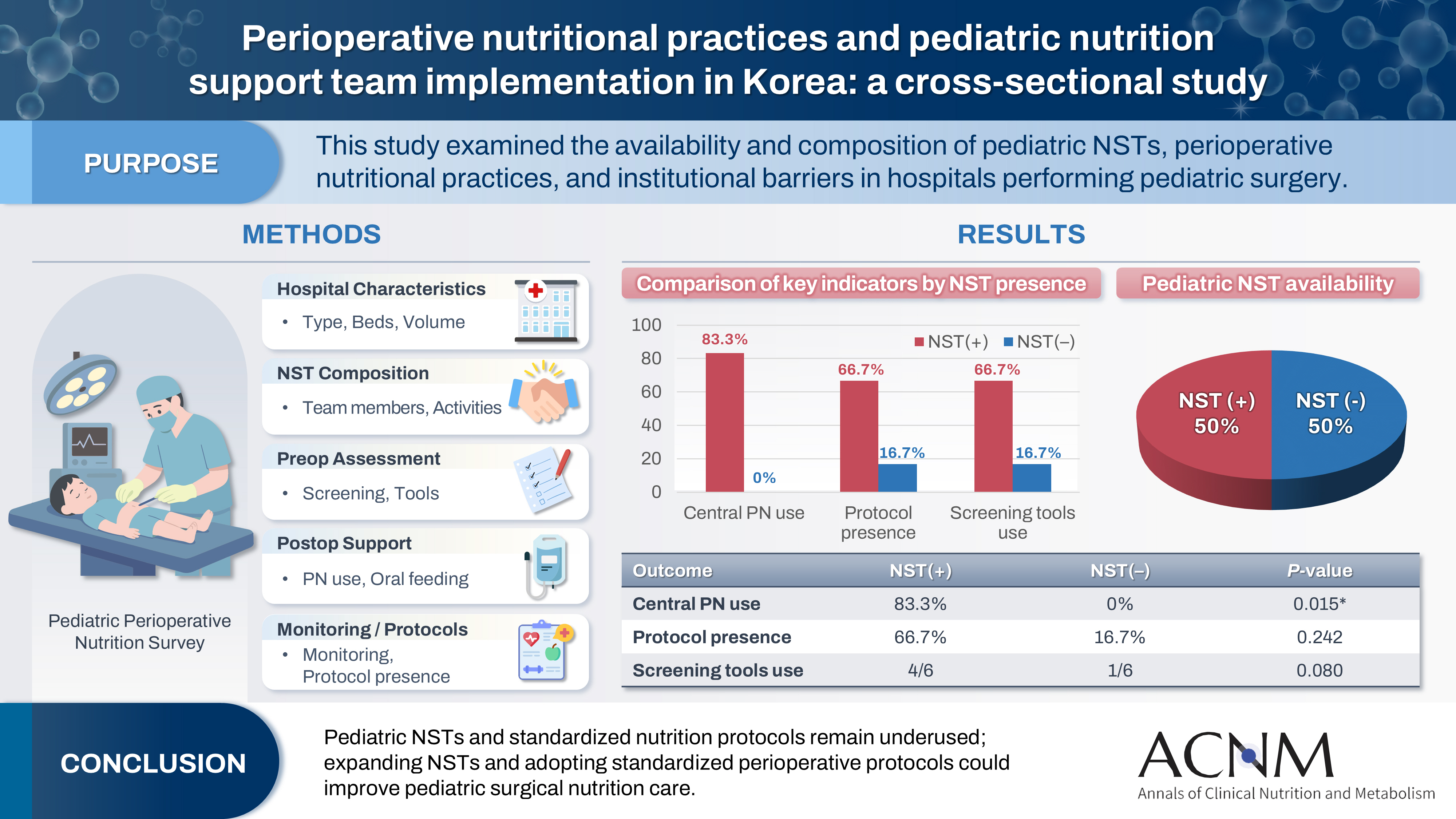
- Purpose
Pediatric surgical patients are vulnerable to perioperative malnutrition, yet standardized nutritional care and structured nutrition support team (NST) involvement remain inconsistent across institutions. Although multidisciplinary nutritional support has gained increasing attention, data on pediatric NST practices within surgical settings in Korea are limited. This study examined the availability and composition of pediatric NSTs, perioperative nutritional practices, and barriers in hospitals performing pediatric surgery.
Methods
A nationwide cross-sectional survey was conducted among tertiary and secondary hospitals that perform pediatric surgery in Korea. The questionnaire assessed hospital characteristics, the presence and composition of pediatric NSTs, perioperative nutritional screening and support practices, monitoring protocols.
Results
A total of 12 hospitals participated. Although all were high-capacity institutions, only half reported having a pediatric NST. Routine preoperative nutritional screening was performed in 50% of hospitals, and validated tools such as Screening Tool for the Assessment of Malnutrition in Pediatrics (STAMP) and Pediatric Yorkhill Malnutrition Score (PYMS) were used in 41.7%. Hospitals with a pediatric NST more frequently had institutional protocols for nutritional evaluation (66.7% vs. 16.7%) and were more likely to administer central venous parenteral nutrition postoperatively (83.3% vs. 0%, P=0.015). Enhanced Recovery After Surgery protocols were implemented in only two hospitals (16.7%). Major barriers to pediatric NST operation included insufficient staffing and time constraints.
Conclusion
Pediatric NSTs and standardized perioperative nutrition protocols remain underutilized in Korean surgical centers. Institutions with a pediatric NST demonstrated more structured nutritional practices. Expanding NST infrastructure and establishing standardized perioperative protocols for pediatric surgical patients may enhance the quality and consistency of nutritional care.
- 159 View
- 8 Download

- Impact of tube feeding after pancreaticoduodenectomy on nutritional intake and status: a retrospective cohort study in Japan
- Masaharu Ishida, Masahiro Iseki, Shuichiro Hayashi, Aya Noguchi, Hideaki Sato, Shingo Yoshimachi, Akiko Kusaka, Mitsuhiro Shimura, Shuichi Aoki, Daisuke Douchi, Takayuki Miura, Shimpei Maeda, Masamichi Mizuma, Kei Nakagawa, Takashi Kamei, Michiaki Unno
- Ann Clin Nutr Metab 2025;17(3):203-209. Published online December 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0020

-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 
- Purpose
Pancreaticoduodenectomy (PD) is one of the most invasive procedures in gastrointestinal surgery. However, the clinical significance of postoperative tube feeding remains unclear. This study investigated the impact of enteral nutrition (EN) on the postoperative nutritional status of patients undergoing PD.
Methods
We retrospectively analyzed 129 patients who underwent PD at Tohoku University Hospital. Nutritional intake and status, evaluated using the Controlling Nutritional Status score, were compared between two groups: an EN group (97 patients) and a non-EN group (32 patients).
Results
There were no significant differences between the two groups in age, sex, body mass index, underlying diseases, operative duration, blood loss, postoperative pancreatic fistula, postoperative complications, delayed gastric emptying, or length of hospital stay. Although the EN group showed improvements in nutritional status both at discharge and compared with preoperative values, none of these changes reached statistical significance. Oral caloric intake was significantly higher in the non-EN group (P=0.01). In contrast, total energy intake was higher in the EN group, but this difference did not reach statistical significance (P=0.07).
Conclusion
Tube feeding after PD did not significantly influence postoperative nutritional status or overall nutritional intake. These findings suggest that EN offers no clear advantage over other approaches; however, further research is warranted to validate these results, refine existing guidelines, and optimize postoperative patient management.
- 144 View
- 8 Download

- Current practices and challenges in nutrition support team activities, 2025 in Korea: a multicenter cross-sectional descriptive study
- So Hyun Nam
- Ann Clin Nutr Metab 2025;17(2):97-103. Published online August 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0026
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Purpose
This study aimed to evaluate the current practices, activities, and challenges of nutrition support teams (NSTs) in Korea. The assessment was conducted as part of the 4th NST Leadership Program of the Korean Society of Surgical Metabolism and Nutrition held in 2025, which seeks to foster leadership and enhance team functionality.
Methods
A nationwide survey was conducted in February 2025 among 54 NST members from 44 institutions. The survey explored team composition, consultation volume, educational programs, barriers to implementation, institutional support, and reimbursement challenges.
Results
Of the 44 participating hospitals, most (86.4%) operated a single NST, with multidisciplinary physician involvement from over three specialties in 77.2% of cases. Inpatient referrals to NSTs were generally low, with less than 10% at 63% of institutions. Only 40.9% had an individual office, and formal incentive systems were reported in 18.1% of hospitals. Educational programs for in-hospital staff were limited (29.5%), and less than half conducted regular academic meetings. Rates of adoption of NST recommendations varied widely, with barriers including a lack of engagement from attending physicians, failure to review the recommendations, and department-specific clinical policies. Efforts to promote NST activation included computerized prescription systems, automated referral workflows, staff education, and quality improvement initiatives. Participants focused on sharing effective NST cases, building incentives, exchanging clinical insights, clarifying team roles and leadership, and developing unified practice guidelines.
Conclusion
NSTs in Korea are well established but face ongoing challenges in collaboration and sustainability. Continued leadership and policy support are crucial for enhancing team performance and improving patient outcomes. -
Citations
Citations to this article as recorded by- Perioperative nutritional practices and pediatric nutrition support team implementation in Korea: a cross-sectional study
Dayoung Ko, Honam Hwang, Hee-Beom Yang, Joong Kee Youn, Hyun-Young Kim
Ann Clin Nutr Metab.2025; 17(3): 181. CrossRef
- Perioperative nutritional practices and pediatric nutrition support team implementation in Korea: a cross-sectional study
- 4,881 View
- 73 Download
- 1 Crossref

Review
- Improving the usability of lipid emulsions and optimizing their user-friendliness: a narrative review
- Keisuke Kubota, Natsuko Ichikawa, Kazuhiro Isoda, Misato Enomoto, Miyoko Kosugi, Mari Tanabe, Naoya Sakuraba, Sayuri Endo, Atsushi Suzuki, Masanori Hashimoto
- Ann Clin Nutr Metab 2025;17(2):104-113. Published online August 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0015
-
 Abstract
Abstract
 PDF
PDF - Purpose
Reluctance to administer lipid emulsions to patients receiving treatment, or as recommended by a nutritional support team, often stems from various restrictions or concerns about potential adverse effects. This paper aims to discuss the appropriate clinical use of lipid emulsions to enhance both patient safety and convenience.
Current concept
We conducted a literature review to assess the importance of nutritional therapy and nutritional intervention, the advantages and disadvantages of lipid-emulsion administration, the current situation in Japan, and differences between lipid formulations. Here, we address issues regarding lipid-emulsion use, including: administration rate, drug mixing, administration in critically ill patients, and early postoperative use. Our findings suggest the following solutions to each issue: although a rate below 0.1 g/kg/hr is generally recommended, faster administration is possible if needed, depending on the case; administration via a piggy tube to basic infusion formulations is unproblematic; second- and third-generation fat emulsions are safe for critically ill patients, though soybean oil should be used with caution; and while fat emulsion administration is feasible immediately after surgery, due to endogenous energy mobilization, it is preferable to initiate administration from the third to fourth postoperative day.
Conclusion
The provisional conclusions of this study are as follows: the introduction of medium-chain triglyceride formulations and fish oil (second- and third-generation lipid emulsions), which are not yet available in Japan, is urgently needed; and individualized administration is essential due to substantial interindividual variability in lipid emulsion usage.
- 3,709 View
- 26 Download

Original Articles
- Evaluation of the modified Nutrition Risk in Critically Ill score in Korean critically ill patients with COVID-19: a retrospective cohort study
- Won Ho Han, Jong-Mog Lee, Jae Hoon Lee, Hyun Mi Lee, Ji-Yeon Kim, Mok Young Jang, Sung-Sik Han
- Ann Clin Nutr Metab 2025;17(2):125-131. Published online August 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0009
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Purpose
We evaluated the efficacy of the modified Nutrition Risk in Critically Ill (mNUTRIC) score for malnutrition screening and its association with mortality in intensive care unit (ICU) patients with COVID-19.
Methods
The nutritional status of 129 COVID-19 ICU patients admitted between February 2021 and May 2022 was assessed using American Society for Parenteral and Enteral Nutrition/Academy of Nutrition and Dietetics (ASPEN/AND) criteria. The sensitivity, specificity, and clinical correlations of the mNUTRIC score were analyzed.
Results
Of the 129 patients, 35 (27.1%) met the ASPEN/AND malnutrition criteria. Multivariable analysis identified the mNUTRIC score, underlying malignancy, and mechanical ventilation as significant factors associated with malnutrition. The mNUTRIC score had a sensitivity of 77.1% and specificity of 63.8% (area under the curve [AUC], 0.71; 95% confidence interval [CI], 0.62–0.79) for diagnosing malnutrition, improving to 88.6% and 80.9%, respectively, after adjusting for malignancy and ventilation (AUC, 0.89; 95% CI, 0.82–0.95). Patients with a low mNUTRIC score had a mortality rate of 2.9% and a median ICU stay of 7.7 days (range, 0–84.2 days), whereas those with a high score (≥5) had a mortality rate of 13.1% and a median ICU stay of 10.2 days (range, 1.4–88.5 days) (P=0.046 and P=0.011, respectively).
Conclusion
The mNUTRIC score is an effective screening tool for malnutrition in ICU patients with COVID-19, especially those with malignancy or requiring mechanical ventilation, and is strongly associated with mortality and length of ICU stay.
- 2,398 View
- 29 Download

- Perioperative outcomes of older adult patients with pancreatic cancer based on nutritional status: a retrospective cohort study
- Takanori Morikawa, Masaharu Ishida, Masamichi Mizuma, Kei Nakagawa, Takashi Kamei, Michiaki Unno
- Ann Clin Nutr Metab 2025;17(1):66-74. Published online April 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.001
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study investigated the effects of preoperative nutritional status on postoperative outcomes in older adult patients with pancreatic adenocarcinoma.
Methods
The background and perioperative factors of patients who underwent pancreatectomy for pancreatic adenocarcinoma between 2007 and 2020 were retrospectively analyzed.
Results
Patients aged 75 years or over (older adults) were significantly associated with hypertension, upfront surgery, and lower prognostic nutritional index. In addition, these patients had a significantly lower rate of portal vein resection, less blood loss, and shorter operation time than patients aged less than 75 years (non-older adults). During the postoperative course, older adult patients had a higher rate of pneumonia and lower overall survival than younger patients, although recurrence‐free survival was comparable. In addition, older adult patients showed preoperative malnutrition as a risk factor for postoperative in‐hospital death.
Conclusion
Surgical treatment for pancreatic cancer in older adult patients was performed safely. However, preoperative malnutrition is a risk factor for in‐hospital death and such patients require nutritional support and less‐invasive surgery. -
Citations
Citations to this article as recorded by- Strengthening collaboration: introducing the contributions of Japanese Society for Surgical Metabolism and Nutrition to Annals of Clinical Nutrition and Metabolism
Ye Rim Chang
Ann Clin Nutr Metab.2025; 17(2): 95. CrossRef
- Strengthening collaboration: introducing the contributions of Japanese Society for Surgical Metabolism and Nutrition to Annals of Clinical Nutrition and Metabolism
- 1,574 View
- 22 Download
- 1 Crossref

- Effects of enteral nutrition formulas with varying carbohydrate amounts on glycemic control in diabetic mice
- Yukari Miki, Kazuo Hino
- Ann Clin Nutr Metab 2025;17(1):85-93. Published online April 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0006
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study evaluated the effects of an 8‑week liquid diets with different carbohydrate contents–64% energy in HINE E‑Gel (ST) and 50% energy in HINE E‑Gel LC (LC)–on glycemic control and nutritional status in a mouse model of type 2 diabetes mellitus (db/db mice). The objective was to determine whether reducing carbohydrate intake within the Dietary Reference Intakes for Japanese people improves glycemic control indices, addressing the evidence gap in regarding the long‑term safety and efficacy of low‑carbohydrate enteral nutrition in patients with diabetes.
Methods
db/db mice (n=10 per group) and non‑diabetic db/m mice (n=4) as controls were fed ST, LC, or AIN‑93G diets ad libitum for 8 weeks. The diets primarily differed in carbohydrate content (64% in ST vs. 50% in LC). Blood glucose and glycated hemoglobin (HbA1c), plasma glucose and glycoalbumin, organ weights, and renal function markers were measured weekly or at 4 and 8 weeks. Histopathological examinations of the liver and kidneys were performed at 8 weeks.
Results
At 8 weeks, the LC group showed significantly lower plasma glucose (P=0.0051) and glycoalbumin (P=0.0013) levels compared to the ST group, with a trend toward lower HbA1c (P=0.0514). Although body weight was significantly higher in the LC group (P=0.0038), there were no significant differences between the ST and LC groups in caloric intake, renal function, or histopathological findings.
Conclusion
Reducing carbohydrate intake to 50% of total energy within dietary guidelines may improve glycemic control in diabetic mice, suggesting the need for further long‑term evaluation for clinical applications. -
Citations
Citations to this article as recorded by- Strengthening collaboration: introducing the contributions of Japanese Society for Surgical Metabolism and Nutrition to Annals of Clinical Nutrition and Metabolism
Ye Rim Chang
Ann Clin Nutr Metab.2025; 17(2): 95. CrossRef
- Strengthening collaboration: introducing the contributions of Japanese Society for Surgical Metabolism and Nutrition to Annals of Clinical Nutrition and Metabolism
- 1,500 View
- 28 Download
- 1 Crossref

Review
- Perioperative nutritional management to improve long-term outcomes in critically ill perioperative organ transplant patients: a narrative review
- Toshimi Kaido
- Ann Clin Nutr Metab 2025;17(1):18-24. Published online April 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0005
-
 Abstract
Abstract
 PDF
PDF - Purpose
This review examines the significance of perioperative nutritional management in organ transplantation, with a particular focus on liver transplantation. Organ transplant recipients often experience malnutrition and sarcopenia due to nutritional and metabolic abnormalities associated with organ dysfunction. Because transplantation is a highly invasive procedure, optimizing perioperative nutritional care is critical for improving short-term outcomes and reducing postoperative infection-related mortality.
Current concept
Recent clinical investigations have shown that liver transplant recipients, who are frequently afflicted with end-stage liver disease and uncompensated cirrhosis, are particularly vulnerable to protein-energy malnutrition and secondary sarcopenia. Our analysis identified low pre-transplant nutritional status and the absence of preoperative branched-chain amino acid supplementation as independent risk factors for post-transplant sepsis. In response, we developed a customized nutritional therapy protocol that incorporates precise body composition analysis, serial measurements of biochemical markers (including prealbumin, zinc, and the branched-chain amino acid/tyrosine ratio), and targeted supplementation with branched-chain amino acids, zinc acetate, and synbiotics. Early initiation of enteral nutrition coupled with postoperative rehabilitative interventions resulted in improved outcomes. In addition, stratified body composition parameters correlated with survival differences and informed revised transplantation criteria.
Conclusion
Tailored perioperative nutritional management and rehabilitative strategies are essential for improving early postoperative outcomes in liver transplantation. These findings underscore the need for proactive nutritional assessment and intervention, which may represent a breakthrough in transplant prognosis. Future research should refine nutritional protocols and integrate novel biomarkers, while education and interdisciplinary collaboration remain crucial for enhancing transplant outcomes and reducing complications. -
Citations
Citations to this article as recorded by- Strengthening collaboration: introducing the contributions of Japanese Society for Surgical Metabolism and Nutrition to Annals of Clinical Nutrition and Metabolism
Ye Rim Chang
Ann Clin Nutr Metab.2025; 17(2): 95. CrossRef
- Strengthening collaboration: introducing the contributions of Japanese Society for Surgical Metabolism and Nutrition to Annals of Clinical Nutrition and Metabolism
- 3,513 View
- 88 Download
- 1 Crossref

Original Article
- The enteral feeding tube access route in esophageal cancer surgery in Japan: a retrospective cohort study
- Hiroyuki Kitagawa, Keiichiro Yokota, Tsutomu Namikawa, Kazuhiro Hanazaki
- Ann Clin Nutr Metab 2025;17(1):58-65. Published online April 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0003

-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 
- Purpose
Feeding catheter jejunostomy is a useful access route for early enteral nutrition during esophageal cancer surgery. However, it may lead to postoperative bowel obstruction associated with feeding jejunostomy (BOFJ). To prevent BOFJ, we introduced feeding catheter duodenostomy via the round ligament in 2018. This study aimed to compare the incidence of BOFJ and postoperative body weight changes between feeding catheter jejunostomy and duodenostomy.
Methods
A total of 109 patients who underwent thoracoscopic esophagectomy and gastric tube reconstruction for esophageal cancer at Kochi Medical School Hospital between March 2013 and November 2020 were included. Preoperative patient characteristics (age, sex, preoperative weight, body mass index, cancer stage, and preoperative treatment), surgical outcomes (operative time, blood loss, and postoperative complications [wound infection, pneumonia, anastomotic leakage, BOFJ]), and body weight changes at 1, 3, 6, and 12 months post-surgery were compared between the jejunostomy (J) and duodenostomy (D) groups.
Results
The D group consisted of 35 patients. No significant differences were observed between the groups regarding age, sex, weight, body mass index, cancer stage, operative time, postoperative complications, or duration of tube placement. However, the D group had a significantly lower rate of preoperative chemotherapy (45.7% vs. 78.4%, P=0.001) and lower operative blood loss (120 mL vs. 150 mL, P=0.046) than the J group. All 12 cases of BOFJ occurred in the J group. Furthermore, the D group experienced a significantly lower weight loss ratio at 1 month postoperatively (93.9% vs. 91.8%, P=0.039).
Conclusion
In thoracoscopic esophagectomy, feeding duodenostomy may prevent bowel obstruction and reduce early postoperative weight loss without increasing operative time compared with feeding catheter jejunostomy. -
Citations
Citations to this article as recorded by- Strengthening collaboration: introducing the contributions of Japanese Society for Surgical Metabolism and Nutrition to Annals of Clinical Nutrition and Metabolism
Ye Rim Chang
Ann Clin Nutr Metab.2025; 17(2): 95. CrossRef
- Strengthening collaboration: introducing the contributions of Japanese Society for Surgical Metabolism and Nutrition to Annals of Clinical Nutrition and Metabolism
- 2,163 View
- 28 Download
- 1 Crossref

Guideline
- A practical guide for enteral nutrition from the Korean Society for Parenteral and Enteral Nutrition: Part I. prescribing enteral nutrition orders
- Ye Rim Chang, Bo-Eun Kim, In Seok Lee, Youn Soo Cho, Sung-Sik Han, Eunjung Kim, Hyunjung Kim, Jae Hak Kim, Jeong Wook Kim, Sung Shin Kim, Eunhee Kong, Ja Kyung Min, Chi-Min Park, Jeongyun Park, Seungwan Ryu, Kyung Won Seo, Jung Mi Song, Minji Seok, Eun-Mi Seol, Jinhee Yoon, Jeong Meen Seo, for KSPEN Enteral Nutrition Committee
- Ann Clin Nutr Metab 2025;17(1):3-8. Published online April 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0002
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study aimed to develop a comprehensive practical guide for enteral nutrition (EN) designed to enhance patient safety and reduce complications in Korea. Under the leadership of the Korean Society for Parenteral and Enteral Nutrition (KSPEN), the initiative sought to standardize EN procedures, improve decision-making, and promote effective multidisciplinary communication.
Methods
The KSPEN EN committee identified key questions related to EN practices and organized them into seven sections such as prescribing, delivery route selection, formula preparation, administration, and quality management. Twenty-one experts, selected based on their expertise, conducted a thorough literature review to formulate evidence-based recommendations. Drafts underwent peer review both within and across disciplines, with final revisions completed by the KSPEN Guideline Committee. The guide, which will be published in three installments, addresses critical elements of EN therapy and safety protocols.
Results
The practical guide recommends that EN orders include detailed elements and advocates the use of electronic medical records for communication. Standardized prescription forms and supplementary safety measures are outlined. Review frequency is adjusted according to patient condition—daily for critically ill or unstable patients and as dictated by institutional protocols for stable patients. Evidence indicates that adherence to these protocols reduces mortality, complications, and prescription errors.
Conclusion
The KSPEN practical guide offers a robust framework for the safe delivery of EN tailored to Korea’s healthcare context. It emphasizes standardized protocols and interdisciplinary collaboration to improve nutritional outcomes, patient safety, and operational efficiency. Rigorous implementation and monitoring of adherence are critical for its success. -
Citations
Citations to this article as recorded by- Bridging evidence and clinical practice: a practical guide for enteral nutrition from the Korean Society for Parenteral and Enteral Nutrition
Suk-Kyung Hong
Ann Clin Nutr Metab.2025; 17(1): 1. CrossRef
- Bridging evidence and clinical practice: a practical guide for enteral nutrition from the Korean Society for Parenteral and Enteral Nutrition
- 6,071 View
- 175 Download
- 1 Crossref

Original Articles
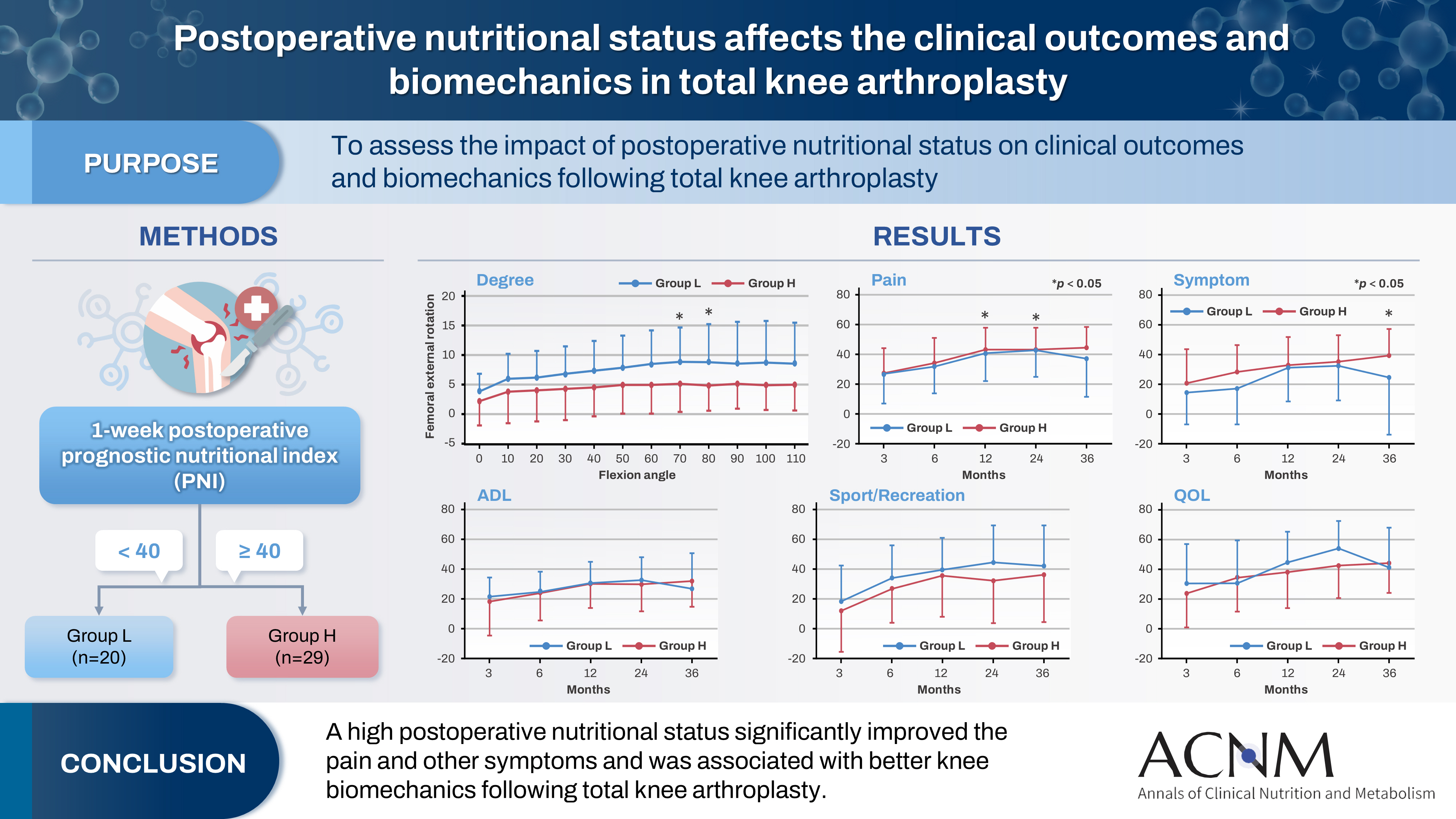
- Impact of postoperative nutritional status on the patients’ clinical outcomes and knee biomechanics following total knee arthroplasty in Japan: a prospective cohort study
- Kenichi Kono, Tetsuya Tomita, Takaharu Yamazaki, Masashi Tamaki, Shuji Taketomi, Ryota Yamagami, Reo Inoue, Yuki Taniguchi, Sakae Tanaka, Kazuhiko Fukatsu
- Ann Clin Nutr Metab 2025;17(1):50-57. Published online April 1, 2025
- DOI: https://doi.org/10.15747/ACNM.24.019
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material 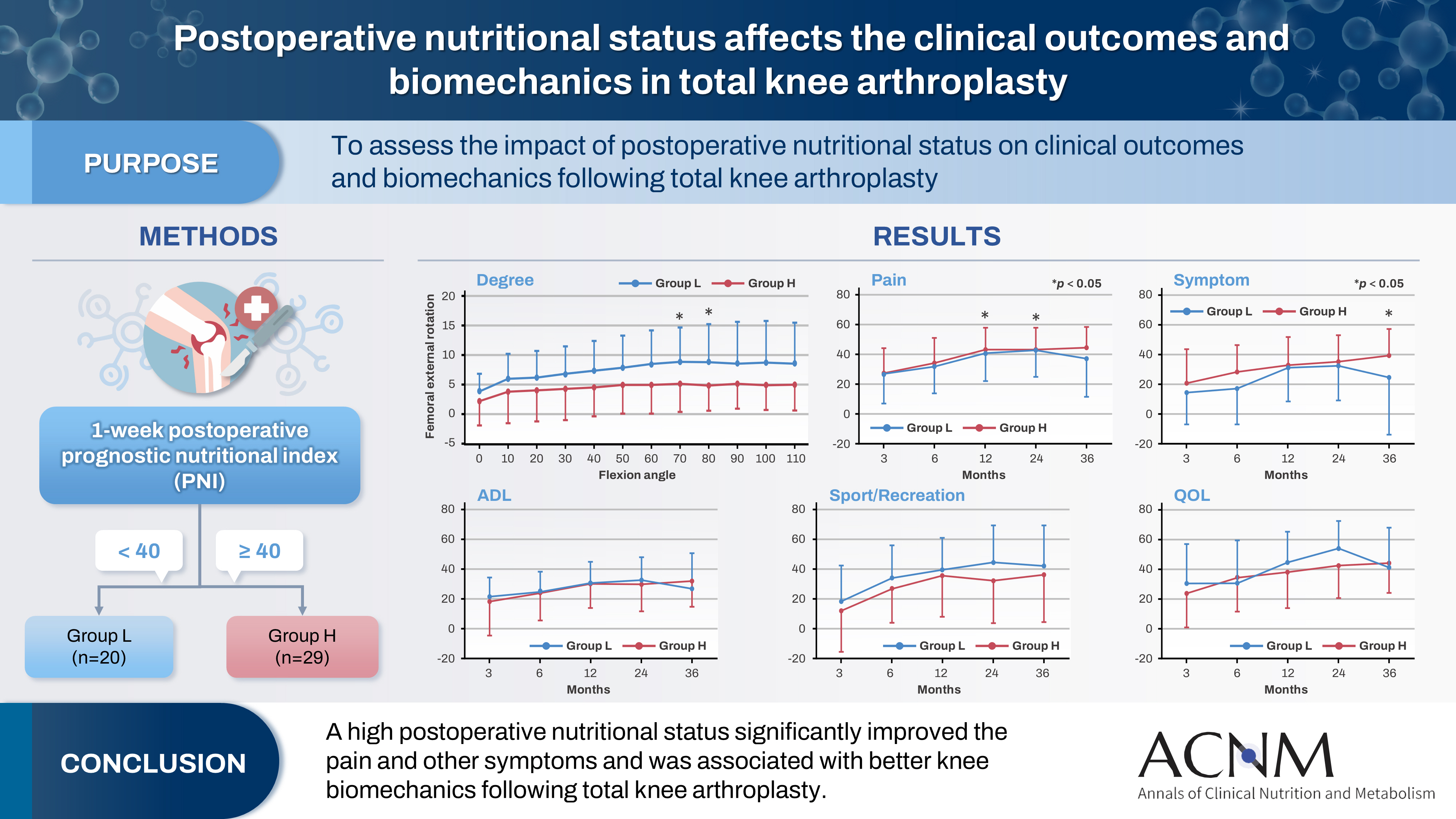
- Purpose
The impact of postoperative nutritional status on clinical outcomes and biomechanics following total knee arthroplasty remains largely unknown. This study aimed to assess this question using the prognostic nutritional index to evaluate the nutritional status of orthopedic participants.
Methods
Patients with knee osteoarthritis who underwent total knee arthroplasty (n=49) in Japan were divided into two groups based on their 1-week postoperative prognostic nutritional index. Group L patients had a prognostic nutritional index <40, whereas Group H comprised patients with a prognostic nutritional index ≥40. Postoperative improvements in Knee Injury and Osteoarthritis Outcome Score were evaluated. The patients performed squats under single-fluoroscopic surveillance in the sagittal plane for biomechanical evaluation. A two-dimensional/three-dimensional registration technique was employed to measure the tibiofemoral kinematics. The axial rotation of the femoral component relative to the tibial component and the anteroposterior translation of the medial and lateral femorotibial contact points were measured.
Results
Group H showed significantly higher pain scores than Group L at 12 and 36 months postoperatively and a significantly higher symptom score at 36 months postoperatively. The kinematic comparison revealed that the axial external rotation in Group L was larger than that in Group H from 70° to 80° with flexion. Moreover, in the medial anteroposterior translation, Group L was more anteriorly located than Group H, with flexion beyond 30°.
Conclusion
The results suggest that a high postoperative nutritional status significantly improved pain and other symptoms and was associated with better knee biomechanics following total knee arthroplasty.
- 2,228 View
- 34 Download

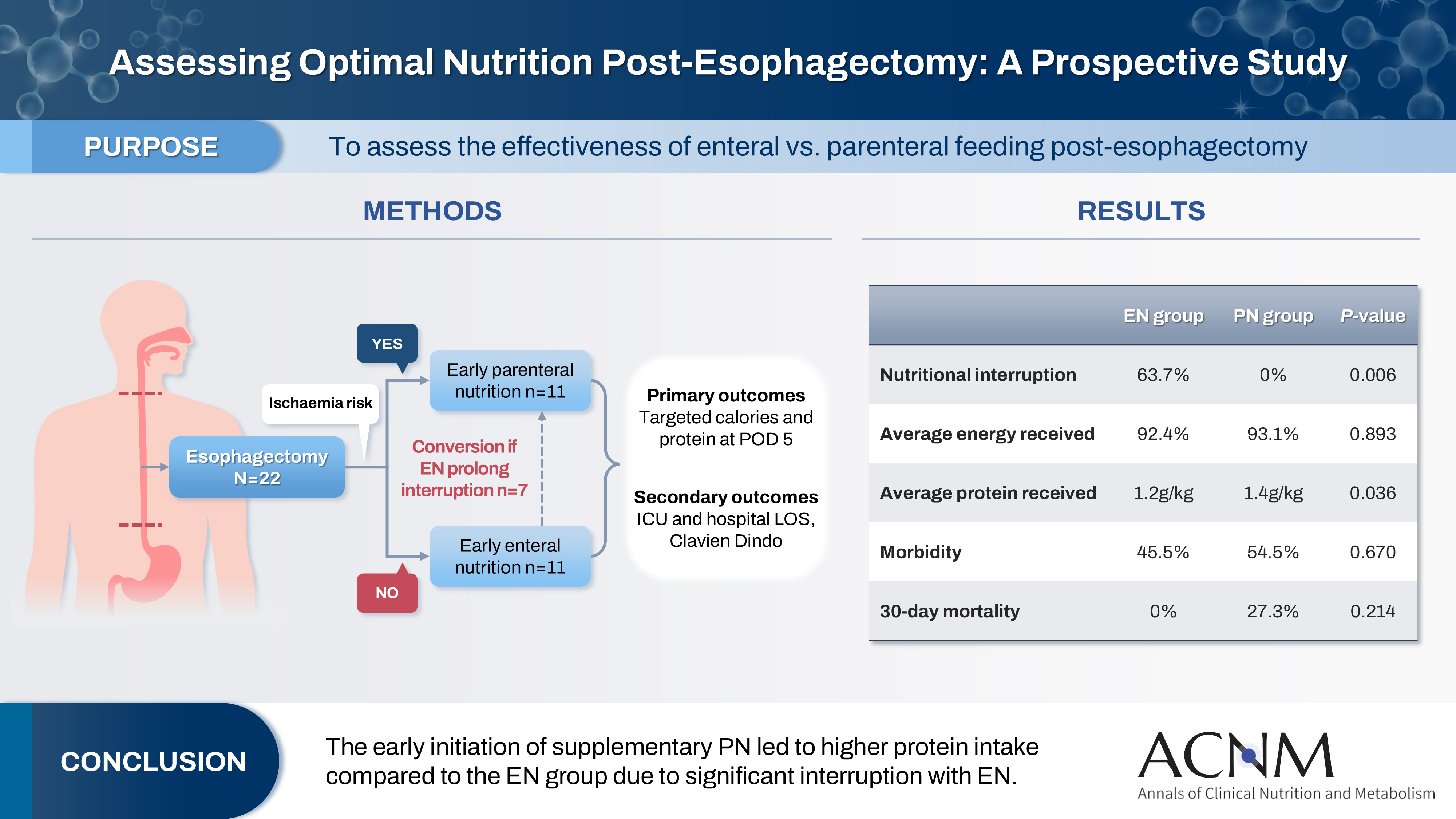
- Comparison of efficacy of enteral versus parenteral nutrition in patients after esophagectomy in Malaysia: a prospective cohort study
- Ramizah Mohd Shariff, Sze Chee Tee, Shukri Jahit Mohammad, Khei Choong Khong
- Ann Clin Nutr Metab 2025;17(1):41-49. Published online April 1, 2025
- DOI: https://doi.org/10.15747/ACNM.24.016
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 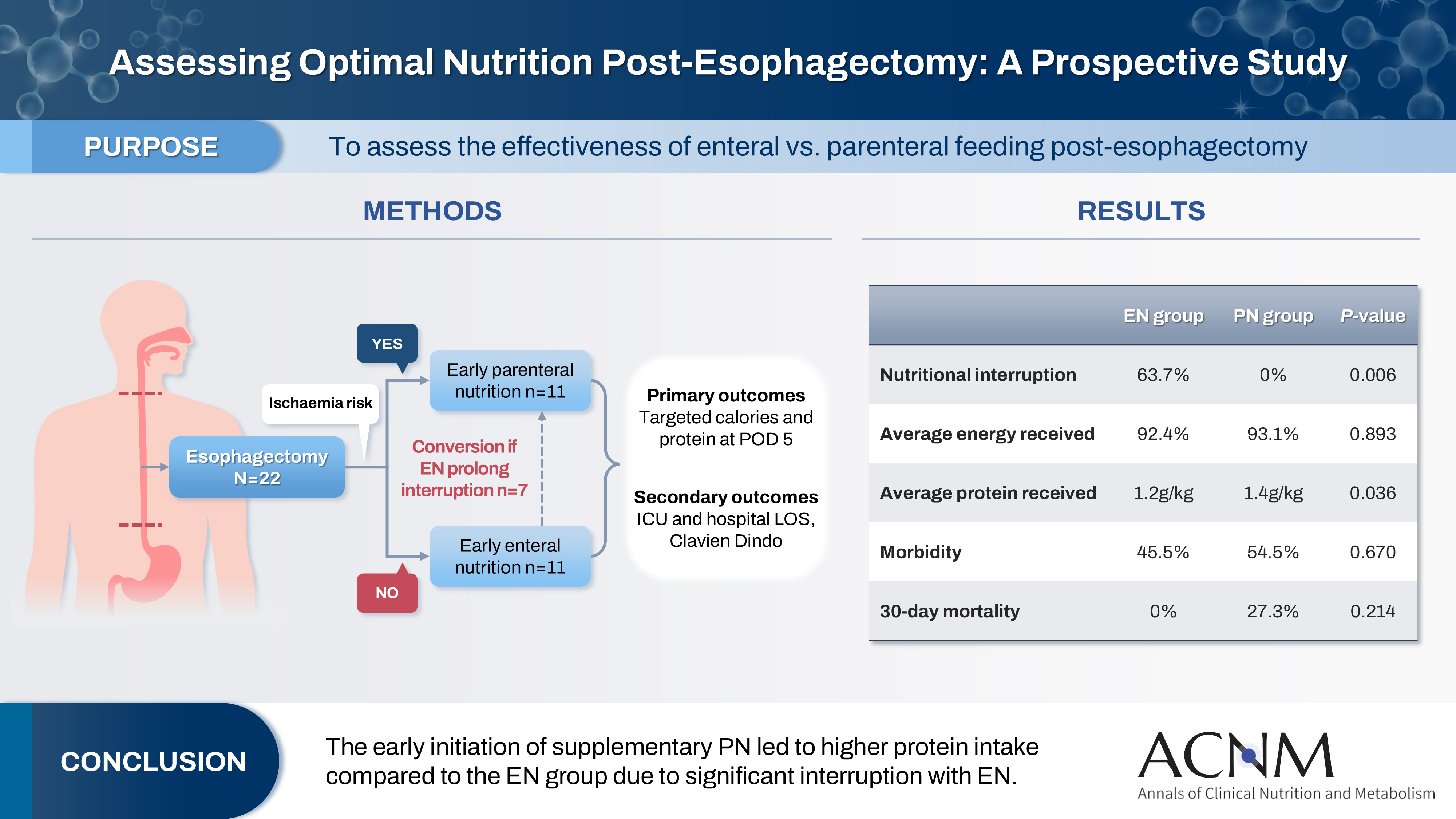
- Purpose
This study aims to assess the effectiveness of enteral versus parenteral feeding in patients after esophagectomy.
Methods
This a prospective cohort study of post-esophagectomy intensive care unit (ICU) patients over 12 months in the National Cancer Institute, Malaysia. Early enteral feeding followed the Enhanced Recovery After Surgery protocol, and parenteral nutrition (PN) was considered if there was a risk for conduit ischemia. It compared the effectiveness of enteral versus PN following esophagectomy, and assessed the correlations between biochemical nutritional markers and hospital lengths of stay or ventilation days.
Results
It included two cohorts receiving PN (n=11) or enteral nutrition (EN) (n=11) following elective esophagectomy. Preoperative weight, body mass index, and Subjective Global Assessment were higher in the EN group (P=0.033, P=0.021, P=0.031, respectively). Nutritional interruption occurred more frequently in the EN group (63.7%) compared to the PN group (P=0.001). Mean levels of energy and protein received were 93.1 kcal/kg and 1.4 g/kg for PN versus 92.4 kcal/kg and 1.2 g/kg for EN (P=0.893, P=0.036). The median lengths of ICU stay (P=0.688) and postoperative stay (P=0.947) between groups showed no significant difference. In addition, 30-day mortality (P=0.214) and other postoperative complications (P>0.05) were comparable in the two groups.
Conclusion
Early initiation of supplementary PN due to significant interruption in EN led to higher protein intake compared to the EN group. However, there were no significant differences in postoperative outcomes, including 30-day mortality, ICU length of stay, and ventilation days. PN ensures adequate nutritional intake, especially in terms of protein delivery, without adversely affecting postoperative recovery and clinical outcomes. -
Citations
Citations to this article as recorded by- Optimizing nutritional support in upper gastrointestinal surgery: A comprehensive review of feeding jejunostomy techniques and outcomes
Ioana Alexandra Prisacariu, Konstantinos Eleftherios Koumarelas, Konstantinos Argyriou, Alexandros Charalabopoulos, Grigorios Christodoulidis
World Journal of Gastrointestinal Surgery.2025;[Epub] CrossRef
- Optimizing nutritional support in upper gastrointestinal surgery: A comprehensive review of feeding jejunostomy techniques and outcomes
- 4,749 View
- 57 Download
- 1 Crossref

Guideline
- Nutritional support for critically ill patients by the Korean Society for Parenteral and Enteral Nutrition — part I: a clinical practice guideline
- Seung Hwan Lee, Jae Gil Lee, Min Kwan Kwon, Jiyeon Kim, Mina Kim, Jeongyun Park, Jee Young Lee, Ye Won Sung, Bomi Kim, Seong Eun Kim, Ji Yoon Cho, A Young Lim, In Gyu Kwon, Miyoung Choi, KSPEN Guideline Committee
- Ann Clin Nutr Metab 2024;16(3):89-111. Published online December 1, 2024
- DOI: https://doi.org/10.15747/ACNM.2024.16.3.89
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Purpose: Nutritional support for adult critically ill patients is essential due to the high risk of malnutrition, which can lead to severe complications. This paper aims to develop evidence-based guidelines to optimize nutritional support in intensive care units (ICUs).
Methods: The Grading Recommendations, Assessment, Development and Evaluation process was used to develop and summarize the evidence on which the recommendations were based. Clinical outcomes were assessed for seven key questions.
Results: We recommend the following: (1) initiate enteral nutrition (EN) within 48 hours after treatment as it is associated with improved outcomes, including reduced infection rates and shorter ICU stays; (2) early EN is preferred over early parenteral nutrition due to better clinical outcomes; (3) the use of supplementary parenteral nutrition to meet energy targets during the first week of ICU admission in patients receiving early EN is conditionally recommended based on patient-specific needs; (4) limited caloric support should be supplied to prevent overfeeding and related complications, particularly in the early phase of critical illness; (5) higher protein intake is suggested to improve clinical outcomes, such as muscle preservation and overall recovery; (6) additional enteral or parenteral glutamine is conditionally recommended against due to the lack of significant benefit and potential harm; and (7) fish oil-containing lipid emulsions is conditionally recommended due to their potential to enhance clinical outcomes, including reduced infection rates and shorter ICU stays.
Conclusion: These evidence-based recommendations can improve clinical outcomes and support healthcare providers in making informed decisions about nutritional interventions in the ICU. -
Citations
Citations to this article as recorded by- Enteral Nutrition Versus a Combination of Enteral and Parenteral Nutrition in Critically Ill Adult Patients in the Intensive Care Unit: An Overview of Systematic Reviews and Meta-Analysis
Paraskevi Papanikolaou, Xenophon Theodoridis, Androniki Papaemmanouil, Niki N. Papageorgiou, Alexandra Tsankof, Anna-Bettina Haidich, Christos Savopoulos, Konstantinos Tziomalos
Journal of Clinical Medicine.2025; 14(3): 991. CrossRef
- Enteral Nutrition Versus a Combination of Enteral and Parenteral Nutrition in Critically Ill Adult Patients in the Intensive Care Unit: An Overview of Systematic Reviews and Meta-Analysis
- 22,555 View
- 517 Download
- 1 Crossref

Original Articles
- The impact of nutritional intervention by a nutrition support team on extrauterine growth restriction in very low birth weight infants in Korea: a retrospective cohort study
- Seung Yun Lee, Hye Su Hwang, Waonsun Im, Hyojoung Kim, Mi Lim Chung
- Ann Clin Nutr Metab 2024;16(3):149-157. Published online December 1, 2024
- DOI: https://doi.org/10.15747/ACNM.2024.16.3.149
-
 Abstract
Abstract
 PDF
PDF - Purpose: Achieving proper weight gain through adequate nutrition is critically important in very low birth weight (VLBW) infants. Despite recent active nutritional interventions, growth restriction is still common in VLBW infants. We aimed to determine whether nutritional intervention by a nutrition support team (NST) mitigated extrauterine growth restriction (EUGR) in VLBW infants.
Methods: We retrospectively reviewed the medical records of VLBW infants admitted to Haeundae Paik Hospital between March 2010 and February 2024. EUGR was defined as a decrease in the weight-for-age-z-score>1.2 from birth to the postconceptional age of 36 weeks, using Fenton growth charts.
Results: Among the 603 enrolled VLBW infants, 434 (72.0%) were diagnosed with EUGR. When comparing the control and nutritional intervention groups, the incidence of EUGR was significantly lower in infants in the intervention group (80.6% vs. 62.8%, P<0.00). Intervention group infants started enteral feeding earlier and reached half and full enteral feeding earlier (P<0.05). In addition, intravenous protein and lipid supply started sooner, increased at a faster rate, and reached peak concentrations sooner in the intervention group (P<0.05).
Conclusion: Nutritional intervention by an NST resulted in a significant decrease in the development of EUGR in VLBW infants.
- 2,369 View
- 52 Download

- Perioperative nutritional practice of surgeons in Korea: a survey study
- Ji-Hyeon Park, Mi Ran Jung, Sang Hyun Kim, Hongbeom Kim, Gyeongsil Lee, Jae-Seok Min, Heung-Kwon Oh, Jung Hoon Bae, Yoona Chung, Dong-Seok Han, Seung Wan Ryu, The External Relation Committee of the Korean Society of Surgical Metabolism and Nutrition
- Ann Clin Nutr Metab 2024;16(3):134-148. Published online December 1, 2024
- DOI: https://doi.org/10.15747/ACNM.2024.16.3.134
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Purpose: Enhanced recovery after surgery (ERAS) protocols advocate reduced fasting and early nutrition to improve recovery in surgical patients. However, data on ERAS implementation among Korean surgeons performing major abdominal surgeries remain sparse.
Methods: A survey conducted by the External Relation Committee of the Korean Society of Surgical Metabolism and Nutrition assessed perioperative nutritional practices among 389 Korean general surgeons from February to September 2023. The survey covered preoperative fasting, carbohydrate drinks, nasogastric tube use, postoperative dietary progression, parenteral nutrition (PN), and oral supplements, yielding 551 responses stratified by specialty.
Results: More than 80% of respondents practiced “midnight NPO (Nil Per Os)” fasting, often at the anesthesiology department’s request, while 70%–80% reported no use of preoperative carbohydrate drinks. Most surgeons began dietary progression with water on postoperative day one, advancing to a liquid or soft diet by day two. PN was routinely prescribed by 49% of respondents, with a common dosage of 1,000–1,500 kcal/d. Oral supplements were selectively provided, with 21% of surgeons prescribing them universally.
Conclusion: The results reveal significant variability in perioperative nutrition practices across Korean surgical specialties, with many adhering to traditional practices despite ERAS guidelines. These findings highlight a need for standardized guidelines in Korea to optimize perioperative nutritional support and improve patient recovery outcomes following major abdominal surgeries. -
Citations
Citations to this article as recorded by- Development of the Korean enhanced recovery after surgery audit program
Soo-Hyuk Yoon, Jae-Woo Ju, Ho-Jin Lee, Jeesun Kim, Min Jung Kim, Ji Won Park, Do Joong Park, Seung Yong Jeong
Scientific Reports.2025;[Epub] CrossRef - Perioperative nutrition practices in gastrointestinal cancer surgery: A nationwide survey among German surgical departments
Rahel Maria Strobel, Katharina Beyer, Johannes Christian Lauscher, Marc Martignoni, Christoph Reißfelder, Tim Vilz, Arved Weimann, Maria Wobith
Langenbeck's Archives of Surgery.2025;[Epub] CrossRef
- Development of the Korean enhanced recovery after surgery audit program
- 5,840 View
- 84 Download
- 2 Crossref

Interesting image
- Pneumothorax due to malpositioned nasogastric enteral feeding tube
- Hyebeen Kim, Suk-Kyung Hong
- Ann Clin Nutr Metab 2024;16(2):87-88. Published online August 1, 2024
- DOI: https://doi.org/10.15747/ACNM.2024.16.2.87
- 1,687 View
- 29 Download

Original Articles
- Impact of immune-supplementation on muscle health and inflammation status of South Indian patients who have undergone gastrointestinal resection: a pilot randomized-controlled study
- Nivedita Pavithran, Catherine Bompart, Alisa Alili, Sudheer Othiyil Vayoth
- Ann Clin Nutr Metab 2024;16(2):78-86. Published online August 1, 2024
- DOI: https://doi.org/10.15747/ACNM.2024.16.2.78
-
 Abstract
Abstract
 PDF
PDF - Purpose: Gastrointestinal (GI) resection significantly impacts nutritional and physical health, causing stress and inflammation that increase energy needs. Post-operative caloric intake often falls short, disrupting protein homeostasis and compromising muscle health. Nutritional supplementation is crucial to reduce inflammation and maintain muscle health. This study aimed to evaluate the impact of a three-week oral nutritional immuno-supplement (IMM) intervention compared to a control (CTL) on post-operative inflammatory status and muscle health in patients receiving limb and chest physiotherapy from June to August 2023.
Methods: A randomized, controlled, blinded cohort of 20 patients (ages 30–75) undergoing GI surgery was established. Participants were recruited on the day of surgery and assigned to either the CTL, which received standard protein supplementation, or the IMM group, which received protein immune-enriched supplementation for three weeks. All participants also received chest and limb physiotherapy. Follow-up and data collection were conducted at three post-surgery time points: 3 days, 7 days, and 3 weeks. Assessments included body composition, handgrip strength, basal metabolic rate, 24-hour dietary intake, and C-reactive protein (CRP) levels.
Results: Fifteen patients completed the study (IMM=9, CTL=6). After three weeks of supplementation, the IMM group showed a significant increase in lean mass percentage and handgrip strength, along with a significant decrease in CRP levels, compared to the CTL.
Conclusion: A 3-week oral immuno-supplement provided to patients post-GI resection, in conjunction with limb and chest physiotherapy, is more effective in reducing inflammation and preserving muscle health compared to standard protein supplementation.
- 1,287 View
- 12 Download

- Early nutritional support for inpatients reduces admission rates to intensive care units in Korea: a single-center case-control study
- Hyun Suk Kim, Jae Do Yang, Se Wung Han, Mi Rin Lee, Da-Sol Kim, Sejin Lee, Seon-Hyeong Kim, Chan-Young Kim
- Ann Clin Nutr Metab 2024;16(2):57-65. Published online August 1, 2024
- DOI: https://doi.org/10.15747/ACNM.2024.16.2.57
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Purpose: Early nutritional support (ENS) for critically ill patients is promoted by many studies. However, there is a lack of data evaluating its necessity in general wards. This study aims to determine the impact of ENS on patients in general wards.
Methods: Patients aged 18 and above, admitted to the Jeonbuk National University Hospital in Jeonju from January 2020 to December 2020, who were eligible for nutritional support and hospitalized for at least 7 days were included in the study. We divided the patients into two groups: the ENS group, who received nutritional support within 48 hours of admission, and the control group, who received it after 48 hours.
Results: Among 1,077 patients, 146 met the inclusion criteria. The ENS group (n=38) and the control group (n=108) were compared retrospectively. There was a significant age difference between the two groups (P=0.028). The admission ratio to the intensive care unit (ICU) in the ENS group was significantly lower than that in the control group (10.2% vs. 26.3%, P=0.019). The calorie support rate (%) and protein support rate (%) in the ENS group were significantly higher than in the control group (50.12%±23.30% vs. 38.56%±18.02%, P=0.006; 44.61%±25.07% vs. 32.07%±22.76%, P=0.002, respectively). After propensity score matching, the ENS was significantly associated with ICU low admissions (odds ratio 0.08, 95% confidence interval 0.01–0.69, P=0.022).
Conclusion: A future multi-center study considering underlying diseases is needed to provide additional scientific evidence to support the effects of ENS.
- 2,103 View
- 24 Download

- Comparative assessment of nutritional characteristics of critically ill patients at admission and discharge from the neurosurgical intensive care unit in Korea: a comparison study
- Eunjoo Bae, Jinyoung Jang, Miyeon Kim, Seongsuk Kang, Kumhee Son, Taegon Kim, Hyunjung Lim
- Ann Clin Nutr Metab 2023;15(3):97-108. Published online December 1, 2023
- DOI: https://doi.org/10.15747/ACNM.2023.15.3.97
-
 Abstract
Abstract
 PDF
PDF - Purpose: Patients in neurosurgical (NS) intensive care units (ICUs) experience considerable energy and protein deficits associated with adverse outcomes. This study aimed to compare the nutritional status of patients at admission to (baseline) and discharge from the NS ICU.
Methods: This was a single-center, retrospective, before and after study of patients admitted in the NS ICU of the CHA Bundang Medical Center, from January 31, 2019, to February 28, 2020. All anthropometric data, biochemical data, clinical data, and dietary data were collected during the NS ICU stay. Specifically, we investigated the cumulative caloric deficit rate, phase angle and skeletal muscle index as indicators of lean muscle mass, and nitrogen balance according to demographic and clinical characteristics.
Results: A total of 140 NS patients were studied. Calf circumference decreased from 31.4±4.2 cm at baseline to 30.2±4.0 cm at discharge (P<0.001). Energy supply rate increased from 44.4% at baseline to 89.2% at discharge. Phase angle (PhA) patients with an modified Nutrition Risk in the Critically ill (mNUTRIC) score≤5 group had significantly lower PhA values than those with an mNUTRIC score>5 (P=0.005).
Conclusion: Although clinical and dietary parameters of patients in the NS ICU improved from baseline to discharge, anthropometric and biochemical markers of lean muscle mass and nutritional status decreased. PhA and nitrogen balance difference values were significantly different between those with an mNUTRIC score≤5 and those with an mNUTRIC score>5. These data indicate that the nutritional risk of critically ill patients increases during hospitalization in the NS ICU. -
Citations
Citations to this article as recorded by- A Review on the Effects of Multiple Nutritional Scores on Wound Healing after Neurosurgery.
Jingqian Ye, Bo Ning , Jianwen Zhi
International Journal of Biology and Life Sciences.2025; 9(2): 82. CrossRef - Transition from Enteral to Oral Nutrition in Intensive Care and Post Intensive Care Patients: A Scoping Review
Gioia Vinci, Nataliia Yakovenko, Elisabeth De Waele, Reto Stocker
Nutrients.2025; 17(11): 1780. CrossRef
- A Review on the Effects of Multiple Nutritional Scores on Wound Healing after Neurosurgery.
- 3,074 View
- 25 Download
- 2 Crossref

- Perioperative nutritional practices and attitudes among gastrointestinal oncologic surgeons in Korea: a nation-wide survey study
- Dae Hoon Kim, Jeong-Meen Seo, Min-Gew Choi
- Ann Clin Nutr Metab 2023;15(3):81-87. Published online December 1, 2023
- DOI: https://doi.org/10.15747/ACNM.2023.15.3.81
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Purpose: This study aimed to investigate the current perioperative nutritional practices and attitudes among gastrointestinal (GI) oncologic surgeons in Korea. Evidence-based perioperative nutritional practices are not well-established in this field.
Methods: A nationwide survey was conducted with 24 items, targeting GI oncologic surgical faculty members from March 2022 to April 2022 through social networking service messaging and email. Whole target number was 3,421.
Results: Out of responding 161 GI surgeons, 83.9% were male and 16.1% were female, and about 49.7% were in their 40s. When asked about their hospital policies, 67.1% reported the existence of formal nutritional screening programs. However, the execution and analysis of these programs varied considerably. Most surgeons conducted preoperative nutritional screening, with albumin testing the most frequently performed. In addition, nutritional supplementation—primarily protein drinks—was given before surgery. The duration for which these supplements were used varied from ≤3 days to 4–7 days. Most respondents recognized the importance of addressing nutritional deficiencies in patients with GI tumors; however, when asked about immunonutrition, 89.4% of surgeons admitted having limited knowledge.
Conclusion: Although there is recognition of the importance of evidence-based nutrition practices in GI and oncologic surgery programs, this study reveals limited implementation of such practices. This study highlights a considerable opportunity to leverage existing positive surgeon beliefs and published data on the benefits of perioperative nutrition to enhance surgical nutrition practices and to improve patient outcomes in Korea.
- 1,257 View
- 8 Download

Review
- Role of nutrition in wound healing and nutritional recommendations for promotion of wound healing: a narrative review
- Myoungjean Ju, Yoonhong Kim, Kyung Won Seo
- Ann Clin Nutr Metab 2023;15(3):67-71. Published online December 1, 2023
- DOI: https://doi.org/10.15747/ACNM.2023.15.3.67
-
 Abstract
Abstract
 PDF
PDF - Purpose: Addressing both malnutrition and wound healing requires strategic intervention. However, guidelines for adequate nutrition for a variety of wounds are lacking. Based on the latest literature review, we summarize the role of nutrition in each stage of wound healing and nutritional recommendations for wound healing.
Current concept: Wounds undergo three healing phases: inflammatory, proliferative, and remodeling. The inflammatory phase involves clotting and cleaning the wound. The proliferative phase builds the wound bed through tissue growth. In the remodeling phase, collagen strength increases. Proper nutrition is crucial throughout. During inflammation, calcium, vitamin K, A, and E, zinc, and proteins are essential. In proliferation, amino acids, B vitamins, lipids, zinc, and iron play key roles. During remodeling, vitamins C and E, zinc, and water are critical for collagen synthesis and skin cell maturation. Vulnerable groups like the elderly, newborns, and obese patients need proper nutrition for skin maintenance. For pressure ulcers with malnutrition risk, recommendations are 30–35 kcal/kg/day energy, 1.25–1.5 g/kg/day protein, and 30 mL/kg water. Supplements might be added if regular meals don’t meet needs. For diabetic foot ulcers, despite common deficiencies, the 2019 International Working Group on the Diabetic Foot advises against prioritizing nutritional interventions over standard care due to limited high-quality evidence.
Conclusion: Despite limited guidelines, nutrition assessment is vital for wound evaluation. A multidisciplinary approach is key, emphasizing nutrition’s role in wound healing. Implementing nutritional interventions tailored to the wound and the individual’s nutritional status is essential. This comprehensive strategy ensures the best wound care outcomes. -
Citations
Citations to this article as recorded by- Electrospun-based nanofibers as ROS-scavenging scaffolds for accelerated wound healing: a narrative review
Mohammad Ebrahim Astaneh, Narges Fereydouni
International Journal of Polymeric Materials and Polymeric Biomaterials.2025; 74(15): 1349. CrossRef - Implementing a screening protocol for food insecure patients within a long‐term acute care hospital (LTACH): A community health needs assessment (CHNA)
Molly MacDonald, Christopher Stimson, Marti Samsel, Tina Gross
Nutrition in Clinical Practice.2025; 40(6): 1598. CrossRef - Nanoformulations Loaded with Phytochemicals for Combating Wound Infections and Promoting Wound Healing: Current Applications and Innovations
Panoraia I. Siafaka, Androulla N. Miliotou, Mehmet Evren Okur, Gökçe Karaotmarlı Güven, Ioannis D. Karantas, Neslihan Üstündağ Okur
Applied Sciences.2025; 15(10): 5413. CrossRef - Combining Topical Oxygen and Negative-Pressure Wound Therapy: New Insights from a Pilot Study on Chronic Wound Treatment
Bartosz Molasy, Mateusz Frydrych, Rafał Kuchciński, Stanisław Głuszek
Journal of Clinical Medicine.2025; 14(15): 5564. CrossRef - Undifferentiated connective tissue dysplasia and skin: what to do? Dietitian’s position
E. A. Nikitina, S. V. Orlova, T. T. Batysheva, N. V. Balashova, M. V. Alekseeva
Medical alphabet.2025; 1(19): 60. CrossRef - Nutritional Immunity in Wound Infection: Unveiling the Role of Dietary Elements in Host–Pathogen Interaction
Chaoming Chen, Xuanfan Hu, Da He, Xuemei He, Lan Shen
Food Science & Nutrition.2025;[Epub] CrossRef - Role of Nutrients and Diet in Wound Healing: The Emerging Paradigm for Effective Therapy
Aishik Banerjee, Arup Ghosh, Subhrajyoty Basu, Soumitra Sahana, Amit Kundu, Sumanta Mondal
Current Indian Science.2025;[Epub] CrossRef - Assessment of energy requirements in patients with obesity: A narrative review
Cagney Cristancho, Kris M. Mogensen, Malcolm K. Robinson
Nutrition in Clinical Practice.2025;[Epub] CrossRef - Lueyang Black‐Boned Chicken and Black Bean Soup Promoting the Acute Healing of Skin Wounds, Accompanying Special Flavor Substances
Mengya Zhao, Zining Luo, Pengyan Tong, Yining Jia, Xin Yang, Jing Liu, Fangyu Long
Food Chemistry International.2025;[Epub] CrossRef - Cancer-Related Malnutrition and Oxidative Stress in Colorectal Cancer Surgery: A Narrative Review of Pathophysiology and Postoperative Outcomes
Andrii Zahorodnii, Alicja Jelska, Paulina Głuszyńska, Hady Razak Hady
Antioxidants.2025; 14(11): 1289. CrossRef - UCI Sports Nutrition Project: The Role of Nutrition in the Prevention and Management of Illnesses and Injuries in Elite Cycling
Patrick B. Wilson, David B. Pyne, Adrian Rotunno
International Journal of Sport Nutrition and Exercise Metabolism.2025; : 1. CrossRef - Clinical Impact of Nutritional Intervention on Pressure Injury Healing in a Paraplegic Patient: A Case Report
Young ran Kim, Mi young Jang, Jun ho Park
Clinical Nutrition Research.2025; 14(4): 241. CrossRef - Impact of Epigenetics, Diet, and Nutrition-Related Pathologies on Wound Healing
John Hajj, Brandon Sizemore, Kanhaiya Singh
International Journal of Molecular Sciences.2024; 25(19): 10474. CrossRef
- Electrospun-based nanofibers as ROS-scavenging scaffolds for accelerated wound healing: a narrative review
- 58,116 View
- 1,526 Download
- 13 Crossref

Original Article
- Consultation pattern changes of parenteral nutrition with a multidisciplinary nutrition support team in a recently opened hospital in Korea: a retrospective cohort study
- Kyoung Won Yoon, Hyo Jin Kim, Yujeong Im, Seul Gi Nam, Joo Yeon Lee, Hyo Gee Lee, Joong-Min Park
- Ann Clin Nutr Metab 2023;15(2):57-63. Published online August 1, 2023
- DOI: https://doi.org/10.15747/ACNM.2023.15.2.57
-
 Abstract
Abstract
 PDF
PDF - Purpose: Parenteral nutrition (PN) is essential for the treatment of patients with malnutrition. The provision of central PN should be recommended by a nutrition support team (NST) made up of a team of experts, even in a newly established hospital. This study sought to evaluate the effectiveness of PN delivered by a multidisciplinary NST in a recently opened hospital.
Methods: This was a retrospective study of the effectiveness of a central PN recommendation pop-up message by the electronic medical record (EMR) software to prompt physicians to either calculate the required calorie and protein intake or consult with the NST. The study period was divided into pre-NST and post-NST based on the time of recruitment of NST-dedicated personnel.
Results: Patients in the 12-week pre-NST period (n=50) and 12-week post-NST period (n=74) were compared retrospectively. Baseline characteristics were not significantly different between the two groups, except for the median Acute Physiology and Chronic Health Evaluation II score (pre-NST group, 8 [interquartile range, IQR 5–15.5] vs. post-NST group, 15 [IQR 9–24], P=0.012) of the 45 patients total admitted to the intensive care unit. The percentage of patients for whom physicians requested a consultation with the NST for central PN was significantly higher in the post-NST group (52.0% vs. 75.7%, P=0.011). There was no significant difference in achievement of nutrition targets or mortality.
Conclusion: Building a multidisciplinary NST may increase awareness of nutritional status and affect the behavior of physicians in recently-opened hospitals.
- 1,696 View
- 10 Download

Reviews
- Role of preoperative immunonutrition in patients with colorectal cancer: a narrative review
- Soo Young Lee, Hyeung-min Park, Chang Hyun Kim, Hyeong Rok Kim
- Ann Clin Nutr Metab 2023;15(2):46-50. Published online August 1, 2023
- DOI: https://doi.org/10.15747/ACNM.2023.15.2.46
-
 Abstract
Abstract
 PDF
PDF - Purpose: Colorectal cancer surgery presents challenges due to surgical stress and immunosuppression, leading to postoperative complications. Nutrition is crucial for colorectal cancer patients who are prone to malnutrition. This study aims to provide a comprehensive review of the role of preoperative immunonutrition in colorectal cancer surgery.
Current concept: Preoperative immunonutrition, consisting of immunonutrients such as arginine, ω-3 fatty acids, and nucleotides, has emerged as a potential strategy to enhance surgical outcomes by modulating immune responses and reducing complications. Current guidelines recommend preoperative oral nutritional supplements for major abdominal surgery and immunonutrition for nutritionally high-risk patients. Meta-analysis have demonstrated significant decreases in infectious complications and hospital stay durations with preoperative immunonutrition. However, limitations such as publication bias and heterogeneity in the previous studies should be considered. Further research should focus on the optimal timing, duration, and amount of immunonutrition; the patient populations that would benefit most; and the integration of immunonutrition into enhanced recovery after surgery protocols.
Conclusion: While preoperative immunonutrition shows promise, additional research is crucial to refine protocols and establish optimal clinical practice utilization. -
Citations
Citations to this article as recorded by- The 2024 Korean Enhanced Recovery After Surgery (ERAS) guidelines for colorectal cancer: a secondary publication
Kil-yong Lee, Soo Young Lee, Miyoung Choi, Moonjin Kim, Ji Hong Kim, Ju Myung Song, Seung Yoon Yang, In Jun Yang, Moon Suk Choi, Seung Rim Han, Eon Chul Han, Sang Hyun Hong, Do Joong Park, Sang-Jae Park
Annals of Coloproctology.2025; 41(1): 3. CrossRef - Efficacy of preoperative immunonutrition in malnourished patients undergoing colorectal cancer surgery: a study protocol for a multicenter randomized clinical trial
Soo Young Lee, Chang Hyun Kim, Gi Won Ha, Soo Yeun Park, In Jun Yang, Jin Soo Kim, Gyung Mo Son, Sung Il Kang, Sung Uk Bae
Trials.2025;[Epub] CrossRef - The 2024 Korean Enhanced Recovery After Surgery guidelines for colorectal cancer
Kil-yong Lee, Soo Young Lee, Miyoung Choi, Moonjin Kim, Ji Hong Kim, Ju Myung Song, Seung Yoon Yang, In Jun Yang, Moon Suk Choi, Seung Rim Han, Eon Chul Han, Sang Hyun Hong, Do Joong Park, Sang-Jae Park
Annals of Clinical Nutrition and Metabolism.2024; 16(2): 22. CrossRef
- The 2024 Korean Enhanced Recovery After Surgery (ERAS) guidelines for colorectal cancer: a secondary publication
- 13,911 View
- 82 Download
- 3 Crossref

- Perioperative nutrition support: a narrative review
- Rajeev Joshi, Asma Khalife
- Ann Clin Nutr Metab 2023;15(2):40-45. Published online August 1, 2023
- DOI: https://doi.org/10.15747/ACNM.2023.15.2.40
-
 Abstract
Abstract
 PDF
PDF - Purpose: Proper nutrition and supplementation are paramount in surgical patients. Suboptimal nutrition status is increasingly recognized as an independent predictor of poor surgical outcomes. The purpose of this review is to highlight the need for nutritional protocols, with an emphasis on perioperative nutrition.
Current concept: Perioperative nutrition support is considered an adjunctive strategy in most centers, although it is proven to be the key in improving surgical outcomes. There is a need to increase the standards and formulate policies and protocols to optimize perioperative nutrition support. Components of perioperative nutrition include nutritional screening and assessment, prehabilitation, preoperative metabolic optimization and carbohydrate loading, postoperative early enteral feeding and perioperative parenteral nutrition, immunonutrition and micronutrients, and oral nutritional supplementation vs. hospital-based kitchen feeds. Supplemental parenteral nutrition becomes valuable when enteral nutrition alone cannot fulfil energy needs. In patients in the surgical intensive care unit who are dealing with hemodynamic instability, high levels of serum lactate unrelated to thiamine deficiency, acidosis, significant liver dysfunction, high blood sugar, and high blood lipid levels, parenteral nutrition must be started with caution. In the post-surgery care ward, it is advisable to administer up to 30 kcal/kg/day and 1.2–2 g/kg/day of protein.
Conclusion: The positive impact of comprehensive nutritional support and the importance of setting and executing standards must be highlighted. Emphasis should be placed on overcoming existing challenges in implementing nutrition therapy in current surgical practice, as better perioperative nutrition supports better surgical outcomes. -
Citations
Citations to this article as recorded by- Nutritional intervention for weight loss in presurgical phase – case study
Ana-Maria Damian
The Romanian Journal of Nutrition.2024; 4(4): 4. CrossRef
- Nutritional intervention for weight loss in presurgical phase – case study
- 23,489 View
- 191 Download
- 1 Crossref

Original Articles
- Effects of nutritional status and support on the survival of COVID-19 patients in a single tertiary-center intensive care unit in Korea: a case-control study
- Na Gyeong Lee, Hye Jin Kim, Ji Gyeong Kang, Do Hyeon Jeon, Mi Seung Kwak, So Hyun Nam
- Ann Clin Nutr Metab 2023;15(1):30-37. Published online April 1, 2023
- DOI: https://doi.org/10.15747/ACNM.2023.15.1.30
-
 Abstract
Abstract
 PDF
PDF - Purpose: It is important to understand the nutritional status of critically ill COVID-19 patients and to provide adequate associated support. We attempted to determine how nutritional status and the amount of nutritional support provided to critically ill patients affect their survival.
Methods: We retrospectively reviewed the medical records of patients admitted to the intensive care unit of Dong-A University Hospital between January and December 2021. We divided the patients into survivors and those who died during COVID-19 treatment and compared and analyzed their clinical parameters, nutrition-related indicators, nutritional status, and nutritional support.
Results: Of 70 patients reviewed, 57 survived. Mortality was higher in the older group (P=0.006). The patients who underwent ventilator, extracorporeal membrane oxygenation, or continuous renal replacement therapy showed higher mortality. Nutritional status at the time of admission and the nutritional requirements did not differ among patient groups. However, the actual amounts of calories (P<0.001) and protein (P=0.019) supplied were lower in the mortality group. Serum C-reactive protein level was higher (P=0.002) and serum albumin level was lower in those who did not survive (P<0.001) compared with surviving patients at discharge.
Conclusion: We did not determine whether the initial nutritional status of patients with COVID-19 affected their survival due to various factors associated with the severity of the disease. However, given the similarities between disease severity and nutritional status at the time of admission, our results indicate that adequate nutritional support can contribute to survival in critically ill COVID-19 patients with pneumonia. -
Citations
Citations to this article as recorded by- The association between enteral nutrition with survival of critical patients with COVID‐19
Maryam Gholamalizadeh, Zahra Salimi, Khadijeh Abbasi Mobarakeh, Zahra Mahmoudi, Shirin Tajadod, Mahdi Mousavi Mele, Farkhondeh Alami, Bojlul Bahar, Saeid Doaei, Sara Khoshdooz, Masoume Rahvar, Somayeh Gholami, Masoume Pourtaleb
Immunity, Inflammation and Disease.2024;[Epub] CrossRef
- The association between enteral nutrition with survival of critical patients with COVID‐19
- 2,375 View
- 6 Download
- 1 Crossref

- Comparison of a volume-based feeding protocol with standard feeding for trauma patients in intensive care units in Korea: a retrospective cohort study
- Juhong Park, Yesung Oh, Songhee Kwon, Ji-hyun Lee, Mihyang Kim, Kyungjin Hwang, Donghwan Choi, Junsik Kwon
- Ann Clin Nutr Metab 2023;15(1):22-29. Published online April 1, 2023
- DOI: https://doi.org/10.15747/ACNM.2023.15.1.22
-
 Abstract
Abstract
 PDF
PDF - Purpose: Although early enteral nutrition for critically ill patients is essential, it is difficult to provide enteral nutrition to trauma patients in early hospitalization stages due to frequent surgeries and examinations. We aimed to identify the effect of achieving early enteral nutrition goals and improving outcomes through a volume-based feeding (VBF) protocol for trauma patients.
Methods: Patients who were admitted to the trauma intensive care units (TICUs) of the Ajou University Hospital from January 2020 to September 2021 and received enteral tube feeding for at least 7 days were studied. An institution-specific VBF protocol was developed, and nurses were trained in its execution. We retrospectively compared outcomes, such as in-hospital mortality and initial nutritional goal achievement, between the new and standard protocols.
Results: Among 2,935 patients, 109 met the inclusion criteria. Of these, 64 patients received nutrition through VBF, with no feeding intolerance symptoms. The VBF group started enteral nutrition approximately 16.9 hours earlier and group achieved 80% of the target calorie and protein intake approximately one day faster than the control group (n=45). The average calorie supply per body weight per day was 4.9 kcal/kg/day more in the VBF group. An increase of 0.2 g/kg/day was also observed in protein uptake. However, mortality and adverse hospital events did not differ between the groups.
Conclusion: The VBF protocol for patients admitted to the TICU increased the initial nutrient supply without risk of feeding intolerance, but there was no improvement in major clinical outcomes, including mortality and adverse hospital events. -
Citations
Citations to this article as recorded by- Early initiation of gastric tube feeding: ultrasound assessment. A prospective interventional study
Islam M. Elbardan, Ahmed A. Alla Ossman, Nada El Kayal, Assem A. ElRazek Abd-Rabih
Research and Opinion in Anesthesia & Intensive Care.2024; 11(4): 270. CrossRef
- Early initiation of gastric tube feeding: ultrasound assessment. A prospective interventional study
- 3,596 View
- 33 Download
- 1 Crossref

Review
- Efficacy of monounsaturated fatty acids in reducing risk of the cardiovascular diseases, cancer, inflammation, and insulin resistance: a narrative review
- Ki Hyun Kim, Yoonhong Kim, Kyung Won Seo
- Ann Clin Nutr Metab 2023;15(1):2-7. Published online April 1, 2023
- DOI: https://doi.org/10.15747/ACNM.2023.15.1.2
-
 Abstract
Abstract
 PDF
PDF - Purpose: The purpose of this review is to explore the potential benefits of monounsaturated fatty acids (MUFAs), specifically those found in olive oil, on weight loss, cardiovascular disease, cancer, inflammation, and insulin resistance. Additionally, this review examines the use of olive oil–based intravenous lipid emulsions (ILEs) in providing parenteral nutrition to patients with diverse needs.
Current concept: MUFAs, found in olive oil, nuts, and some animal foods, have been found to have numerous health benefits. A diet high in MUFAs can aid in weight loss and reduce the risk of cardiovascular disease. Olive oil, in particular, has been linked to a lower risk of cancer, inflammation, and insulin resistance. In addition, olive oil–based ILEs have been utilized for over two decades and are well tolerated by patients requiring parenteral nutrition.
Conclusion: A diet rich in MUFAs, specifically from olive oil, can provide numerous health benefits, including weight loss and reducing the risk of cardiovascular disease, cancer, inflammation, and insulin resistance. Additionally, olive oil–based ILEs have been shown to effectively provide nutrients to diverse populations requiring parenteral nutrition and have demonstrated the ability to preserve immune function and induce less lipid peroxidation than other ILEs. Further research is needed to fully understand the potential benefits of MUFAs and olive oil-based ILEs, but current evidence suggests that they may be a valuable addition to a healthy diet and medical treatment. -
Citations
Citations to this article as recorded by- The impact of Lactiplantibacillus plantarum on the cream composition: Insight into changes of vitamin D3 content and fatty acid composition
Tetiana Dyrda-Terniuk, Viorica Railean, Aleksandra Bogumiła Florkiewicz, Justyna Walczak-Skierska, Mateusz Kolankowski, Joanna Rudnicka, Dorota Białczak, Paweł Pomastowski
International Dairy Journal.2025; 161: 106118. CrossRef - Palmitoleic and oleic fatty acids as biomarkers for coronary heart disease: A predictive model
Guangzhou Wang, Lin Zhou, Zhengfang Wang, Asmaa Ali, Liang Wu
Irish Journal of Medical Science (1971 -).2025; 194(1): 59. CrossRef - Effects of daily extra virgin olive oil consumption on biomarkers of inflammation and oxidative stress: a systematic review and meta-analysis
Jéssica Vidal Damasceno, Anderson Garcez, Andressa Anelo Alves, Isabella Rosa da Mata, Simone Morelo Dal Bosco, Juliano Garavaglia
Critical Reviews in Food Science and Nutrition.2025; : 1. CrossRef - Macrophages: their role in immunity and their relationship with fatty acids in health and disease
Mayte Rueda-Munguía, Luis Alberto Luévano-Martínez, Gerardo García-Rivas, Elena Cristina Castillo, Omar Lozano
Frontiers in Immunology.2025;[Epub] CrossRef - Evaluation of the Nutritional Value of Prunus dulcis Blossoms and the Antioxidant Compounds of Their Extracted Oil Using Green Extraction Method
Theodoros Chatzimitakos, Vassilis Athanasiadis, Konstantina Kotsou, Ioannis Makrygiannis, Eleni Bozinou, Stavros I. Lalas
Applied Sciences.2024; 14(5): 2001. CrossRef - Oleic Acid and Succinic Acid: A Potent Nutritional Supplement in Improving Hepatic Glycaemic Control in Type 2 Diabetic Sprague–Dawley Rats
Kemmoy G. Lattibeaudiere, Ruby Lisa Alexander-Lindo, Mozaniel Oliveira
Advances in Pharmacological and Pharmaceutical Sciences.2024;[Epub] CrossRef
- The impact of Lactiplantibacillus plantarum on the cream composition: Insight into changes of vitamin D3 content and fatty acid composition
- 30,949 View
- 83 Download
- 6 Crossref

Case Reports
- Development of Wernicke’s Encephalopathy during Total Parenteral Nutrition Therapy without Additional Multivitamin Supplementation in a Patient with Intestinal Obstruction: A Case Report
- Cheong Ah Oh
- Ann Clin Nutr Metab 2022;14(2):93-96. Published online December 1, 2022
- DOI: https://doi.org/10.15747/ACNM.2022.14.2.93
-
 Abstract
Abstract
 PDF
PDF - Wernicke’s encephalopathy (WE) is a serious neurological disorder that can be fatal if not properly treated. In this current paper, I present the case of a 51-year-old male with a perivesical fistula between a presacral abscess and the rectus abdominis muscle. He received total parenteral nutrition therapy during a fasting period because of small bowel obstruction and later developed WE. The patient’s WE-related symptoms improved following rapid treatment with high doses of thiamine.
- 2,889 View
- 29 Download

- Refeeding Syndrome after Gastrectomy in a Patient with Hypophosphatemia: A Case Report
- Cheong Ah Oh
- Ann Clin Nutr Metab 2022;14(2):88-92. Published online December 1, 2022
- DOI: https://doi.org/10.15747/ACNM.2022.14.2.88
-
 Abstract
Abstract
 PDF
PDF - This study describes an 81-year-old male who was highly suspicious for refeeding syndrome (RFS) after a retrospective review of his postoperative clinical progression. This highlights the importance of clinicians’ awareness of the possibility of RFS development in surgical patients with any RFS risk factors.
- 2,114 View
- 20 Download

Original Article
- Provision of Enteral Nutrition in the Surgical Intensive Care Unit: A Multicenter Prospective Observational Study
- Chan-Hee Park, Hak-Jae Lee, Suk-Kyung Hong, Yang-Hee Jun, Jeong-Woo Lee, Nak-Jun Choi, Kyu-Hyouck Kyoung
- Ann Clin Nutr Metab 2022;14(2):66-71. Published online December 1, 2022
- DOI: https://doi.org/10.15747/ACNM.2022.14.2.66
-
 Abstract
Abstract
 PDF
PDF - Purpose: Timely enteral nutrition (EN) is important in critically ill patients. However, use of EN with critically ill surgical patients has many limitations. This study aimed to analyze the current status of EN in surgical intensive care units (ICUs) in South Korea.
Materials and Methods: A multicenter, prospective, observational study was conducted on patients who received EN in surgical ICUs at four university hospitals between August 2021 and January 2022.
Results: This study included 125 patients. The mean time to start EN after admission to the surgical ICU was 6.2±4.6 days. EN was provided to 34 (27.2%) patients within 3 days after ICU admission. At 15.7±15.9 days, the target caloric requirement was achieved by 74 (59.2%) patients through EN alone. Furthermore, 104 (83.2%) patients received supplemental parenteral nutrition after a mean of 3.5±2.1 days. Only one of the four hospitals regularly used enteral feeding tubes and post-pyloric feeding tubes.
Conclusion: Establishing EN guidelines for critically ill surgical patients and setting an appropriate insurance fee for EN-related devices, such as the feeding pump and enteral feeding tube, are necessary.
- 3,526 View
- 31 Download

Review Articles
- Selection of the Enterostomy Feeding Route in Enteral Nutrition
- Dong-Seok Han
- Ann Clin Nutr Metab 2022;14(2):50-54. Published online December 1, 2022
- DOI: https://doi.org/10.15747/ACNM.2022.14.2.50
-
 Abstract
Abstract
 PDF
PDF - Enteral nutrition has several physiologic advantages. For example, it can reduce complications, result in immunological improvement, and prevent bacterial translocation by maintaining the integrity of the intestinal barrier. Enteral tube feeding has a major role in nutritional support of patients with swallowing disorders caused by stroke or other neurologic disorders, neoplasms of the upper digestive tract, and benign esophageal stricture. This review article aimed to present the current knowledge on the clinical application of enteral tube feeding. Especially, based on a literature search on PubMed using the index terms of enteral tube feeding; the indications, advantages, and disadvantages; and insertion methods of various enteral tubes were identified.
- 5,810 View
- 39 Download

- Liver Cirrhosis and Sarcopenia
- Hye Yeon Chon, Tae Hee Lee
- Ann Clin Nutr Metab 2022;14(1):2-9. Published online June 1, 2022
- DOI: https://doi.org/10.15747/ACNM.2022.14.1.2
-
 Abstract
Abstract
 PDF
PDF - Malnutrition is one of the most common complications in patients with liver cirrhosis. In previous studies, cirrhotic patients with severe malnutrition have been associated with higher morbidity and mortality rates before and after liver transplantation. Frailty and sarcopenia are phenotypes of severe malnutrition that have been associated with complications requiring hospitalization or mortality during the wait for transplantation in patients with cirrhosis. Tools for evaluating frailty include the Activities of Daily Living scale, the Karnofsky Performance Status scale, and the Liver Frailty Index. Diagnosed by using computed tomography, sarcopenia is measured with the skeletal muscle index at L3 and is normalized by height. Nutritional status should be evaluated within the first 24~48 hours of hospitalization in every patient with cirrhosis. Among the various available screening tools, the Royal Free Hospital-Nutritional Prioritizing Tool proposed in the UK is recommended. Nutritional counseling with a multidisciplinary team is recommended to improve long-term survival in patients with cirrhosis. Multidisciplinary nutrition management should include evaluating nutritional status and providing guidance for achieving nutritional goals. Most guidelines suggest a calorie intake of 25~35 kcal/kg/day, and the recommended protein intake is 1.2~1.5 g/kg/day. One beneficial technique for patients is to divide the total recommended intake across four to five daily meals, including a nighttime snack. The principles of nutritional intervention in cirrhotic patients are not different from those in noncirrhotic patients. For improvement of sarcopenia, a strategic approach including physical activity and exercise, hormone replacement therapy, ammonia-lowering agents, and treatment of underlying liver disease is required.
- 9,464 View
- 48 Download

Original Articles
- Clinical Significance of Malnutrition Risk in Severe Trauma Patients: A Single-Center Study
- Hohyun Kim, Kum-Hee Hong, Inah Choi, Kyung-A Lee, Geun Am Song
- Ann Clin Nutr Metab 2021;13(2):68-74. Published online December 31, 2021
- DOI: https://doi.org/10.15747/ACNM.2021.13.2.68
-
 Abstract
Abstract
 PDF
PDF - Purpose: A suboptimal nutritional status is often observed among hospitalized patients across all medical/surgical specialties. The objective of the present study was to (1) analyze the prevalence of malnutrition in severe trauma patients and (2) evaluate the relationship between malnutrition and select clinical outcomes.
Materials and Methods: This retrospective study was conducted between October 2015 and March 2017 at the Pusan National University Hospital Trauma Center. Of a total of 3,560 patients, 945 were enrolled in this study. Patients were checked for malnutrition using a nutrition assessment tool by the hospital nutrition support team. The parameters assessed included serum albumin, the ratio of actual body weight to ideal body weight (%), total lymphocyte count, appetite, and gastrointestinal problems. Clinical outcomes under consideration included 1) mortality, 2) length of hospitalization, and 3) length of stay in the intensive care unit (ICU).
Results: The total prevalence of malnutrition in hospitalized trauma patients was 55.0% (n=520). Malnutrition risk was the independent prognostic factor of mortality in severe trauma patients (adjusted odds ratio [OR]=3.440; 95% confidence interval [CI]=1.401~8.447, P=0.007). Risk factors of malnutrition were age over 65 years (adjusted OR=2.393; 95% CI=1.699~3.370, P<0.001), injury severity score (adjusted OR=1.034, 95% CI=1.012~1.056, P=0.002), length of hospitalization (adjusted OR=1.104; 95% CI=1.007~1.020, P<0.001), and length of stay in the ICU (adjusted OR=1.050; 95% CI=1.029~1.072, P<0.001).
Conclusion: Malnutrition is widespread in hospitalized patients with severe trauma and results in suboptimal clinical outcomes. Thus, patients at high risk of malnutrition should be monitored carefully during hospitalization.
- 1,839 View
- 20 Download

- Comparison of Post-Operative Nutritional Status according to the Extent of Gastrectomy and the Reconstruction Method in Patients with Gastric Cancer
- Kyung Hwan Kim, Jong Hyuk Yoon, Geum Jong Song, Myoung Won Son, Sung Yong Kim, Moo Jun Baek, Moon Soo Lee
- Ann Clin Nutr Metab 2021;13(2):34-42. Published online December 31, 2021
- DOI: https://doi.org/10.15747/ACNM.2021.13.2.34
-
 Abstract
Abstract
 PDF
PDF - Purpose: Malnutrition is the main complication after gastrectomy and the degree may vary depending on the extent of resection. This study sought to help determine an appropriate type of resection and provide methods for addressing malnutrition after gastrectomy.
Materials and Methods: We retrospectively reviewed medical records of patients with gastric cancer who underwent radical resection at the Soonchunhyang University Cheonan Hospital between December 2012 and December 2013. A total of 100 patients were screened, and all patients were followed for 1 to 3 years. Among this group, 12 underwent total gastrectomy, 5 underwent proximal gastrectomy, 46 underwent distal gastrectomy with Billroth I anastomosis, and 37 with Billroth II anastomosis. The nutritional status assessment included body weight, body mass index, serum albumin, serum hemoglobin, vitamin B12, ferritin, and Nutritional Risk Index (NRI).
Results: Patients who underwent total gastrectomy had lower hemoglobin and vitamin B12 levels compared to patients who underwent distal gastrectomy. The NRI was statistically significantly lower in patients who underwent total gastrectomy than patients who underwent distal gastrectomy. Patients who underwent total gastrectomy had lower vitamin B12 than patients who underwent proximal gastrectomy till the second year after gastrectomy. Regarding postdistal gastrectomy reconstruction, there was no statistically significant difference between the Billroth I and Billroth II groups.
Conclusion: This study showed that patients who underwent total gastrectomy were more susceptible to malnutrition than those who underwent distal or proximal gastrectomy. Patients who undergo gastrectomy should be monitored carefully for nutritional status and given appropriate nutritional support in the post-operative period. -
Citations
Citations to this article as recorded by- Development and Internal/External Validation of a Prediction Model for Weight Loss Following Gastric Cancer Surgery: A Multicenter Retrospective Study
Ji-Hyeon Park, Seong-Ho Kong, Do Joong Park, Han-Kwang Yang, Jong Won Kim, Ki Bum Park, In Cho, Sun-Hwi Hwang, Dong-Wook Kim, Su Mi Kim, Seung-Wan Ryu, Seong Chan Gong, Pil Young Jung, Hoon Ryu, Sung Geun Kim, Chang In Choi, Dae-Hwan Kim, Sung-IL Choi, Ji
Annals of Clinical Nutrition and Metabolism.2022; 14(2): 55. CrossRef
- Development and Internal/External Validation of a Prediction Model for Weight Loss Following Gastric Cancer Surgery: A Multicenter Retrospective Study
- 2,795 View
- 9 Download
- 1 Crossref

- Effect of Malnutrition Assessed by Comprehensive Nutritional Screening Tool on In-Hospital Mortality after Surgery for Gastrointestinal Perforation
- Seung-Young Oh, Hannah Lee, Ho Geol Ryu, Hyuk-Joon Lee
- Surg Metab Nutr 2021;12(1):1-6. Published online June 30, 2021
- DOI: https://doi.org/10.18858/smn.2021.12.1.1
-
 Abstract
Abstract
 PDF
PDF - Purpose: This study examined the effects of malnutrition on in-hospital mortality after surgery for gastrointestinal (GI) perforation.
Materials and Methods: Patients who underwent surgery for GI perforation between 2010 and 2017 were analyzed retrospectively. The preoperative nutritional status was assessed by the Seoul National University Hospital-Nutrition Screening Index, a tool that comprehensively evaluates 11 factors that reflect the nutritional status. The risk factors for in-hospital mortality after surgery for GI perforation were evaluated by univariate and multivariate analyses.
Results: Four hundred and eighty-nine patients were divided into two groups: 439 patients in the survival group and 50 patients in the in-hospital mortality group. The risk of malnutrition was higher (93.6% vs. 65.9%, P<0.001) in the in-hospital mortality group than in the survival group. The preoperative albumin level was lower, and the blood urea nitrogen level was higher in the in-hospital mortality group than in the survival group. Emergency surgery, lymphoma as a cause of perforation, and fecal-contaminated ascites were also identified as factors associated with in-hospital mortality. Multivariate analyses demonstrated that a high risk of malnutrition (HR=5.71, 95% CI 1.38~26.02, P=0.017), lymphoma as a cause of perforation (HR=4.12, 95% CI 1.17~14.51, P=0.028), low preoperative albumin (HR=4.77, 95% CI 2.35~9.69, P<0.001), and high preoperative BUN (HR=1.03, 95% CI 1.01~1.05, P=0.001) had significant effects on the in-hospital mortality after surgery for GI perforation.
Conclusion: A high risk of malnutrition assessed by the composite index was associated with in-hospital mortality after surgery for a GI perforation. -
Citations
Citations to this article as recorded by- Performance of the comprehensive nutrition screening index in predicting mortality after cardiac surgery
Jaeyeon Chung, Jinyoung Bae, Seyong Park, Dong Hyouk Kim, Youn Joung Cho, Karam Nam, Yunseok Jeon, Jae-Woo Ju
Scientific Reports.2024;[Epub] CrossRef - Efficacy of nutritional support protocol for patients with pressure ulcer: comparison of before and after the protocol
Hye Young Woo, Seung-Young Oh, Leerang Lim, Hyunjae Im, Hannah Lee, Ho Geol Ryu
Nutrition.2022; 99-100: 111638. CrossRef
- Performance of the comprehensive nutrition screening index in predicting mortality after cardiac surgery
- 1,508 View
- 8 Download
- 2 Crossref

Review Article
- Perioperative Nutritional Support
- Seung Jong Oh
- J Clin Nutr 2021;13(1):7-11. Published online June 30, 2021
- DOI: https://doi.org/10.15747/jcn.2021.13.1.7
-
 Abstract
Abstract
 PDF
PDF - Malnutrition in surgical patients is a prevalent problem. As the geriatric population gradually increases, surgeons need to be more careful in preventing the risk of iatrogenic malnutrition. Delayed wound healing, exposure to infection, pressure sores, gastrointestinal bacterial overgrowth, and immunosuppression in malnourished patients can be prevented or diminished with active nutritional support. Preoperative nutritional assessment and support, as well as adequate postoperative nutrition, will improve surgical outcomes, which in turn will lead to fewer postoperative complications, shorter hospital stays, and lower medical costs. The success of surgery depends not only on technical surgical skills but also on metabolic interventions that take into account the patient’s ability to deliver the metabolic load and provide adequate nutritional support.
- 765 View
- 2 Download

Original Article
- Impact of Visceral Fat Area Measured by Bioelectrical Impedance Analysis on Clinico-Pathologic Outcomes of Colorectal Surgery
- Kyeong Eui Kim, Woo Jin Song, Minji Seok, Sung Uk Bae, Woon Kyung Jeong, Seong Kyu Baek
- J Clin Nutr 2021;13(1):17-23. Published online June 30, 2021
- DOI: https://doi.org/10.15747/jcn.2021.13.1.17
-
 Abstract
Abstract
 PDF
PDF - Purpose: This study investigated the relationship between the visceral fat area (VFA) and clinico-pathological outcomes in patients with colorectal cancer (CRC).
Methods: This retrospective study included 204 patients who underwent anthropometric measurement by bioelectrical impedance analysis (BIA) before surgical treatment for CRC between January 2016 and June 2020.
Results: According to the average value of the visceral fat area, 119 (58.3%) patients had a low visceral fat area, and 85 (59.1%) patients had a high visceral fat area. Patients with visceral obesity showed a higher BMI compared to patients without visceral obesity, (21.8±1.9 vs. 25.7±2.5, P<0.001). There was no significant difference in the overall perioperative outcomes including total operation time, time to gas out, sips of water, soft diet, hospital stay, and morbidity between patients in the low and high VFA groups. We divided patients into two subgroups according to the degree of cancer progression and more advanced cases with low VFA showed significantly more total and positive retrieved lymph nodes (LNs) (20.9±10.3 vs. 16.1±7.1, P=0.021 and 3.3±2.9 vs. 2.2±2.3, P=0.019, respectively) and a higher proportion of more than 12 retrieved LNs compared to patients with a high VFA (95.1% vs. 90.0%, P=0.047). Body composition analysis showed that phase angle, muscle composition, and body fluid composition were not statistically different between the two groups. However, body fat mass was statistically higher in the high VFA group (22.0±4.6 vs. 12.8±3.1, P<0.001).
Conclusion: Visceral obesity measured by BIA showed lower total and positive retrieved LNs and was not associated with adverse peri-operative outcomes, inflammatory and nutritional, and pathologic outcomes for CRC.
- 1,226 View
- 3 Download

Review Article
- Nutritional Management in Dementia
- Juhee Kang
- J Clin Nutr 2021;13(1):1-6. Published online June 30, 2021
- DOI: https://doi.org/10.15747/jcn.2021.13.1.1
-
 Abstract
Abstract
 PDF
PDF - With the increase in lifespan, and consequent increase in the elderly population, the prevalence of dementia is also increasing. The prevalence of dementia in the elderly over 65 in Korea was 10.3% in 2020 and is expected to increase to 16.1% by 2050. Dementia is a cognitive decline that affects eating behavior, leading to weight loss and malnutrition. In fact, the prevalence of malnutrition has been rising, and has been reported to be 58.9% among dementia patients in community facilities. Dementia requires the intake of sufficient calories and protein to prevent weight loss. On the other hand, intake of certain nutrients, such as omega-3 fatty acids, thiamine, vitamin E, selenium, and copper, helps prevent dementia in healthy people but has no effect on patients with advanced dementia. As dementia worsens, if food intake is reduced, oral nutritional supplements and enteral nutrition should be initiated to prevent weight loss and malnutrition. Dementia patients are very vulnerable to malnutrition, and hence require more active nutritional support.
-
Citations
Citations to this article as recorded by- Development of 3D Printed Snack-dish for the Elderly with Dementia
Ji-Yeon Lee, Cheol-Ho Kim, Kug-Weon Kim, Kyong-Ae Lee, Kwangoh Koh, Hee-Seon Kim
Korean Journal of Community Nutrition.2021; 26(5): 327. CrossRef
- Development of 3D Printed Snack-dish for the Elderly with Dementia
- 1,689 View
- 22 Download
- 1 Crossref

Original Articles
- Characteristics and Practice of Parenteral Nutrition in Hospitalized Adult Cancer Patients in Korea
- Hyo Jung Park, You Min Sohn, Jee Eun Chung, Jung Tae Kim, Jin A Yang, Hye Jung Bae, Ye Won Sung, Sun Hwa Kim,Ji Yoon Cho, Kyung Mi Jung, Hee Kyung Bae
- J Clin Nutr 2020;12(2):34-40. Published online December 31, 2020
- DOI: https://doi.org/10.15747/jcn.2020.12.2.34
-
 Abstract
Abstract
 PDF
PDF - Purpose: There have been no clinical studies on the characteristics of parenteral nutrition (PN) for adult cancer inpatients in South Korea. The published evidence describing modern PN practices in these patients is also extremely limited. Therefore in this retrospective multicenter cross-sectional study, we aimed to investigate the PN support practice in hospitalized adult cancer patients.
Methods: The study included adult cancer patients hospitalized in nine hospitals in South Korea and received PN, during the period from August 1st, 2017 to October 30th, 2017. We evaluated the relevant hospital-based PN practices in this group.
Results: Among the 11,580 inpatient admissions during this period, 759 cancer patients received PN (6.6%). The majority of enrolled patients (97.2%) used commercially available PN and 71.2% of these used peripheral PN formulations. The average in-hospital PN duration was 16.1±19.9 days. Patients received only 65.4±25.4% calories of the recommended target calories. The in-hospital mortality of enrolled patients was 26.1%.
Conclusion: We conclude that commercial PN is the most common form of PN administered to hospitalized adult cancer patients and the overall in-hospital mortality in the patients using PN is higher in South Korea compared to other countries.
- 825 View
- 5 Download

- Effect of Nutritional Intervention by the Nutrition Support Team on Postnatal Growth in Preterm Infants
- So Jin Yoon, Joo Hee Lim, Soon Min Lee, Sun Jung Kim, Sun Kyung Lee, Soo Min Lee
- J Clin Nutr 2020;12(2):26-33. Published online December 31, 2020
- DOI: https://doi.org/10.15747/jcn.2020.12.2.26
-
 Abstract
Abstract
 PDF
PDF - Purpose: Nutritional intervention by an interdisciplinary nutrition support team (NST) can potentially improve postnatal growth outcomes in preterm infants. This study aimed to measure the growth impact of a nutritional intervention package performed by an NST in a quality improvement effort in a neonatal intensive care unit (NICU).
Methods: Fifty-two infants born below 2,000 g and admitted to NICU participated in the Quality Improvement (QI) program between March 2016 and February 2017. The nutritional intervention was applied according to newly established nutritional guidelines on parenteral and enteral nutrition, and an NST performed a weekly nutritional assessment. The Z-scores of weight, height, and head circumference were calculated according to the gestational age and sex. The clinical impact on postnatal growth was compared between the QI and pre-QI groups. The pre-QI group included 69 infants admitted in the same NICU between 2014 and 2015.
Results: The time to the initiation of enteral nutrition decreased significantly (P<0.001). Changes in weight (P=0.027), head circumference (P=0.003), Z-scores between birth, and 40 weeks postconceptional age (PCA) were significantly larger in the QI than the pre-QI group. The percentage of infants weighing below the 10th percentile at one month after birth and at 40 weeks PCA was higher in the pre-QI than the QI group.
Conclusion: The implementation of evidence-based best practices for preterm nutrition resulted in significant improvements in the growth outcomes in preterm infants. -
Citations
Citations to this article as recorded by- Nutrition Supply and Growth Post Nutrition Support Team Activity in Neonatal Intensive Care Unit
Hye Min Ha, Yu Jin Jung, Yoo Rha Hong, So Yoon Choi
Pediatric Gastroenterology, Hepatology & Nutrition.2024; 27(5): 313. CrossRef
- Nutrition Supply and Growth Post Nutrition Support Team Activity in Neonatal Intensive Care Unit
- 1,017 View
- 1 Download
- 1 Crossref

Review Article
- Nutritional Support and Wound Healing
- Chi-Min Park
- J Clin Nutr 2020;12(2):21-25. Published online December 31, 2020
- DOI: https://doi.org/10.15747/jcn.2020.12.2.21
-
 Abstract
Abstract
 PDF
PDF - Wound healing is a coordinated process of sequential events consisting of four phases: hemostasis, inflammation, proliferation, and remodeling. Many factors can affect each phase of this process and have a harmful or beneficial effect on wound healing. Nutrition is closely associated with the wound healing process and is one of the major influencing factors on the outcomes of wound healing. Malnutrition and nutrient deficiencies could adversely affect wound healing and delay it. Many kinds of nutrients can enhance the healing process. Physicians should always assess every patient’s nutritional status to determine nutritional deficiencies. This will enable supplementation, thereby enhancing wound healing. Herein, we review the relationship between nutrition and wound healing, and the effects and mechanisms of each nutrient that is closely related to the wound healing process.
- 732 View
- 9 Download

Original Articles
- Nutritional Status of Patients with Hepatobiliary-Pancreatic Surgical Disease
- Sang Soo Eom, Yong Chan Shin, Chang-Sup Lim, In Woong Han, Woohyun Jung, Yoonhyeong Byun, Dong Wook Choi, Jin Seok Heo, Hongbeom Kim
- Surg Metab Nutr 2020;11(2):46-52. Published online December 30, 2020
- DOI: https://doi.org/10.18858/smn.2020.11.2.46
-
 Abstract
Abstract
 PDF
PDF - Purpose: This study examined the nutritional status of patients with hepatobiliary-pancreatic diseases before surgery to establish basic reference data.
Materials and Methods: This study evaluated retrospectively 2,322 patients admitted for hepatobiliary-pancreatic surgery between 2014 and 2016 at four Korean medical institutions using the body mass index (BMI) score. The prognostic nutrition index (PNI) was calculated in patients diagnosed with malignant diseases.
Results: The mean BMI was 24.0 kg/m2 (range, 13.2~39.1 kg/m2). The patients were classified as low BMI (<21.5 kg/ m2, below 25 percentile), intermediate BMI (21.5~25.5 kg/m2), and high BMI (>25.5 kg/m2, above 75 percentile). There were significant differences in the age, sex distribution, ASA classification, type of hospitalization, biliary drainage, organ, and pathology diagnosis between the pairs among the low, intermediate, and high BMI groups. Among the three BMI groups, the complication rate of the low BMI group was highest (34.4% vs. 29.7% vs. 25.8% P=0.005). The median lengths of hospital stay in the low, intermediate, and high BMI groups were 9, 9, and 7 days, respectively (P<0.001). Multivariate analysis revealed the risk factors of the low BMI group to be a higher ASA classification, biliary drainage, pancreatic disease, and malignant disease. The group with PNI<45 had significantly longer hospital stays than the group with PNI≥45 (P<0.001).
Conclusion: Patients with a low BMI had a higher ASA classification, preoperative biliary drainage, pancreatic disease, and malignant disease. The low PNI group had significantly longer hospital stays than the high PNI group. Screening of the preoperative nutritional status is necessary for assessing the risk of malnutrition and its treatment. -
Citations
Citations to this article as recorded by- Machine learning-based prediction model for post-ERCP cholangitis in patients with malignant biliary obstruction: a retrospective multicenter study
Hengwei Jin, Xu Sun, Chang Fu, Changqing Fan, Junhong Chen, Ziyu Zhang, Yibo Yang, Xiaoyu Fan, Ye He, Siyuan Yin, Kai Liu
Surgical Endoscopy.2025; 39(8): 5107. CrossRef
- Machine learning-based prediction model for post-ERCP cholangitis in patients with malignant biliary obstruction: a retrospective multicenter study
- 1,097 View
- 15 Download
- 1 Crossref

- Clinical Impact of Preoperative Sarcopenia to Postoperative Prognosis in Patients with Periampullary Malignancy: Retrospective Multicenter Study
- Jee Hyun Park, Youngju Ryu, So Hee Song, Naru Kim, Sang Hyun Shin, Jin Seok Heo, Dong Wook Choi, Woo Kyoung Jeong, Woo Hyun Jung, Yong Chan Shin, Chang-Sup Lim, In Woong Han
- Surg Metab Nutr 2020;11(2):40-45. Published online December 30, 2020
- DOI: https://doi.org/10.18858/smn.2020.11.2.40
-
 Abstract
Abstract
 PDF
PDF - Purpose: This study compared the preoperative nutritional status between sarcopenic and non-sarcopenic patients and examined the effects of sarcopenia on the prognosis after a pancreatoduodenectomy (PD).
Materials and Methods: From 2015 to 2016, 480 patients who underwent PD with periampullary cancer at Samsung Medical Center, Seoul National University Boramae Medical Center, Ilsan Paik Hospital, and Ajou University Hospital were analyzed retrospectively. Sarcopenia was measured from the cross-sectional visceral fat and muscle area on CT imaging using an automatic calculation program. The dysnutritional grade was assessed according to Controlling Nutritional Status (CONUT) score system.
Results: Preoperative serum albumin (3.9 g/dl) and cholesterol levels (161.7 mg/dl) of sarcopenic patients were significantly lower than those of the non-sarcopenia patients (4.0 g/dl, P=0.024; 176.1 mg/dl, P=0.005). The proportion of moderate-to-severe dysnutritional grade in sarcopenic patients was significantly higher than in the non-sarcopenic patients (20.0 vs. 8.1%, P=0.004). A comparison of the changes in albumin between before and after PD showed a decrease in sarcopenic patients (0.06 vs. 0.05, P=0.024). Sarcopenia itself was not a factor affecting the overall survival (OS) negatively, but moderate-to-severe dysnutritional grade was an independent risk factor for OS (HR 2.418, CI 1.424~4.107, P=0.001).
Conclusion: Patients with sarcopenia showed poorer preoperative nutritional status than those without sarcopenia, and the sarcopenia affected the postoperative nutritional status negatively. No direct correlation was observed between sarcopenia and OS, but the dysnutritional grade was an independent risk factor that affects OS. As a result, patients with sarcopenia could be affected indirectly for survival because of their poor nutritional status.
- 459 View
- 0 Download

- Nutritional Support Team Approach Decreases the In-Hospital Mortality Rate after Deceased Donor Liver Transplantation
- Sang-Oh Yun, Jong Man Kim, Sangjin Kim, Jinsoo Rhu, Hyun Jung Kim, Soo Hyun Park, Hyo Jung Park, Eunmi Gil, Wonseok Kang, Gyu-Seong Choi, Won Hyuck Chang, Jeong-Meen Seo, Jae-Won Joh
- Surg Metab Nutr 2020;11(1):7-11. Published online June 30, 2020
- DOI: https://doi.org/10.18858/smn.2020.11.1.7
-
 Abstract
Abstract
 PDF
PDF - Purpose: This study compared the mortality rates between a period of time without employing a nutritional support team (NST) and a period of time with an NST.
Materials and Methods: Forty-six patients underwent adult deceased donor liver transplantation (DDLT) in 2016, and their medical records were prospectively collected. All the donor recipients underwent routine enteral feeding after liver transplantation. An NST cared for twenty-one patients after September 2016. The NST consisted of transplant surgeons, hepatologists, a critical care team, a rehabilitation team, dietitians, pharmacists, and nurses. We defined the patients within the time period without an NST as the control group and those patients within the time period with an NST as the case group.
Results: There were no statistically significant differences in baseline or perioperative characteristics between the two groups. The median model for the end-stage liver disease (MELD) score was 36 (range: 21∼40) for the control group and 36 (range: 23∼40) for the case group (P=0.596). The 30-day mortality rate was 24.0% (6/25) for the control group, but it was 4.8% (1/20) for the case group. The patient survival rates at 1-year and 2-year were 68.0% and 64.0% in the control group and 85.7% and 81.0% in the case group, respectively. However, there were no statistically significant differences of the 30-day mortality rate and 1∼2 year patient survival rate between the two groups.
Conclusion: The present study suggests that an NST should be required to prevent 30-day mortality and increase patient survival of adult DDLT patients with a high MELD score.
- 806 View
- 0 Download

- Analysis of the Factors Related to the Incidence and Aggravation of Pressure Ulcers for in Patients from a Nutritional and Clinical Perspective
- Yoon Young Choi, Han Mo Yoo, Young Hwa Kim, Jeong Goo Kim
- Surg Metab Nutr 2020;11(1):16-21. Published online June 30, 2020
- DOI: https://doi.org/10.18858/smn.2020.11.1.16
-
 Abstract
Abstract
 PDF
PDF - Purpose: The incidence of pressure ulcers has reached significant proportions in ward patients. Considering the increasing proportion of older patients, it is important to know the factors associated with pressure ulcers. The purpose of this study was to investigate the association between nutritional status patients and the prognosis of pressure ulcers.
Materials and Methods: Four hundred patients who had their nutritional status evaluated from December 2015 to May 2016 at Daejeon St. Mary’s Hospital were enrolled in this study. The Modified NRS 2002 was used to address the nutritional status. Pressure ulcers were evaluated using the PUSH score, and the nutritional factors were evaluated with pressure ulcer aggravation.
Results: Among the 400 patients who had their nutritional status evaluated, 174 (43.5%) had a pressure ulcer. A high risk of malnutrition was associated significantly with the incidence of pressure ulcers. In patients with pressure ulcers, the necessity of a nutritional support team approach (odds ratio [OR], 2.43; 95% confidence interval [CI], 1.21∼4.91; P=0.01) and the number of pressure ulcers (odds ratio [OR], 3.79; 95% confidence interval [CI], 1.81∼7.91; P<0.001) were risk factors for pressure ulcer aggravation.
Conclusion: These results indicate that a proper evaluation of the malnutrition state and obtaining a nutritional support team intervention are important for preventing the aggravation of pressure ulcers. Furthermore, if a patient has multiple sites of pressure ulcers, a careful assessment will be needed to prevent their deterioration. -
Citations
Citations to this article as recorded by- A Longitudinal Investigation of Stage 2 Pressure Injury Outcomes With Machine Learning Technique to Identify Relevant Factors
Jae Hyung Jeon, Jaewoo Chung, Nam-Kyu Lim
Advances in Skin & Wound Care.2025; 38(9): E81. CrossRef
- A Longitudinal Investigation of Stage 2 Pressure Injury Outcomes With Machine Learning Technique to Identify Relevant Factors
- 646 View
- 5 Download
- 1 Crossref

- Analysis of Muscle Using CT Anthropometry in Major Trauma Patients
- Hang Joo Cho, Yunsup Hwang, Yoon Hyun Lee, Dae Hyun Cho, Dae-Sang Lee, Maru Kim
- Surg Metab Nutr 2020;11(1):12-15. Published online June 30, 2020
- DOI: https://doi.org/10.18858/smn.2020.11.1.12
-
 Abstract
Abstract
 PDF
PDF - Purpose: The feasibility of nutritional assessment using computed tomography anthropometry has been previously proven. The abdominal muscle at the L3 vertebra is a well-known nutritional biomarker for predicting the prognosis of various diseases, and especially sarcopenia. However, any studies on nutritional assessment of the brain, face, or neck via computed tomography are still scarce. We retrospectively investigated the applicability of the masseter muscle as a nutritional biomarker.
Materials and Methods: Patients who underwent simultaneous brain and abdominopelvic computed tomography at a regional trauma center were retrospectively analyzed. Their masseter muscles at 2 cm below the zygomatic arch and abdominal muscle at L3 were assessed via computed tomography anthropometry. Basic clinical data including trauma information was also reviewed. The data was analyzed in conjunction with the patients’ mortality.
Results: A total of 411 patients were analyzed in the study (316 men and 95 women, mean age: 50.41 years, mean areas of the masseter and abdominal muscles: 10.6 and 137.3 cm2, respectively) and there 146 major trauma patients with an injury severity score higher than 15. The masseter muscle area was decreased in the mortality group of major trauma patients (10.4 vs 7.9 cm2, P=0.001). However, abdominal muscles did not show statistical significance (137.9 vs. 117.7 cm2, P=0.054).
Conclusion: The masseter muscle, when analyzed via computed tomography anthropometry, showed a statistical association with patients’ mortality and it could prove its feasibility as a nutritional biomarker.
- 535 View
- 1 Download

- Status of Nutritional Support after Emergency Gastrointestinal Surgery in Korea: Retrospective Multicenter Study
- Dae Sang Lee, Young Eun Park, Kyoung Hoon Lim, Ye Rim Chang, Suk-Kyung Hong, Minchang Kang, Jung-Min Bae, Ji Young Jang, Young Goun Jo, Ki Hoon Kim, Gil Jae Lee
- Surg Metab Nutr 2020;11(1):1-6. Published online June 30, 2020
- DOI: https://doi.org/10.18858/smn.2020.11.1.1
-
 Abstract
Abstract
 PDF
PDF - Purpose: Surgery itself causes an inflammatory response to an injury to the patient that leads to a stress metabolic state. Emergency gastrointestinal surgery may cause complications, such as ileus, bowel obstruction, ischemia, or anastomotic leakage, resulting in a delayed oral diet or poor overall nutrition. This study investigated the route of nutrition for patients who underwent emergency gastrointestinal surgery and when to provide nutrition after surgery.
Materials and Methods: Ten hospitals collected data retrospectively on the nutritional status and nutritional status of patients undergoing emergency gastrointestinal surgery for one year from January to December 2016. The clinical outcomes of the nutrient supply method, duration of supply, and type of surgery were performed. The dates from the time of surgery to the start of enteral nutrition, oral nutrition, and parenteral nutrition were calculated.
Results: Of 706 patients, there were 187 (26.5%) trauma patients, of which 63.5% were male. The onset of nutrition began after an average of 10.7 days postoperatively and after an average of 12.1 days of enteral nutrition. On average, it took 7.7 days to provide adequate calories, of which 63.3% had achieved adequate calories within a week. In the case of minimally invasive surgery, such as laparoscopic surgery, the adequate calorie supply time was five days, which was reached within one week.
Conclusion: In a retrospective multicenter analysis, the patients who underwent emergency gastrointestinal surgery had a late start of oral or enteral nutrition, and the ratio of adequate calorie supply within a week was low.
- 525 View
- 2 Download


 E-submission
E-submission KSPEN
KSPEN KSSMN
KSSMN ASSMN
ASSMN JSSMN
JSSMN
 First
First Prev
Prev


