Indexed in:
Scopus, KCI, KoreaMed
Scopus, KCI, KoreaMed

Previous issues
- Page Path
- HOME > Browse articles > Previous issues
Editorial
- Strengthening collaboration: introducing the contributions of Japanese Society for Surgical Metabolism and Nutrition to Annals of Clinical Nutrition and Metabolism
- Ye Rim Chang
- Ann Clin Nutr Metab 2025;17(2):95-96. Published online August 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0022
- 1,051 View
- 14 Download

Original Article
- Current practices and challenges in nutrition support team activities, 2025 in Korea: a multicenter cross-sectional descriptive study
- So Hyun Nam
- Ann Clin Nutr Metab 2025;17(2):97-103. Published online August 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0026
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Purpose
This study aimed to evaluate the current practices, activities, and challenges of nutrition support teams (NSTs) in Korea. The assessment was conducted as part of the 4th NST Leadership Program of the Korean Society of Surgical Metabolism and Nutrition held in 2025, which seeks to foster leadership and enhance team functionality.
Methods
A nationwide survey was conducted in February 2025 among 54 NST members from 44 institutions. The survey explored team composition, consultation volume, educational programs, barriers to implementation, institutional support, and reimbursement challenges.
Results
Of the 44 participating hospitals, most (86.4%) operated a single NST, with multidisciplinary physician involvement from over three specialties in 77.2% of cases. Inpatient referrals to NSTs were generally low, with less than 10% at 63% of institutions. Only 40.9% had an individual office, and formal incentive systems were reported in 18.1% of hospitals. Educational programs for in-hospital staff were limited (29.5%), and less than half conducted regular academic meetings. Rates of adoption of NST recommendations varied widely, with barriers including a lack of engagement from attending physicians, failure to review the recommendations, and department-specific clinical policies. Efforts to promote NST activation included computerized prescription systems, automated referral workflows, staff education, and quality improvement initiatives. Participants focused on sharing effective NST cases, building incentives, exchanging clinical insights, clarifying team roles and leadership, and developing unified practice guidelines.
Conclusion
NSTs in Korea are well established but face ongoing challenges in collaboration and sustainability. Continued leadership and policy support are crucial for enhancing team performance and improving patient outcomes. -
Citations
Citations to this article as recorded by- Perioperative nutritional practices and pediatric nutrition support team implementation in Korea: a cross-sectional study
Dayoung Ko, Honam Hwang, Hee-Beom Yang, Joong Kee Youn, Hyun-Young Kim
Ann Clin Nutr Metab.2025; 17(3): 181. CrossRef
- Perioperative nutritional practices and pediatric nutrition support team implementation in Korea: a cross-sectional study
- 5,350 View
- 80 Download
- 1 Crossref

Reviews
- Improving the usability of lipid emulsions and optimizing their user-friendliness: a narrative review
- Keisuke Kubota, Natsuko Ichikawa, Kazuhiro Isoda, Misato Enomoto, Miyoko Kosugi, Mari Tanabe, Naoya Sakuraba, Sayuri Endo, Atsushi Suzuki, Masanori Hashimoto
- Ann Clin Nutr Metab 2025;17(2):104-113. Published online August 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0015
-
 Abstract
Abstract
 PDF
PDF - Purpose
Reluctance to administer lipid emulsions to patients receiving treatment, or as recommended by a nutritional support team, often stems from various restrictions or concerns about potential adverse effects. This paper aims to discuss the appropriate clinical use of lipid emulsions to enhance both patient safety and convenience.
Current concept
We conducted a literature review to assess the importance of nutritional therapy and nutritional intervention, the advantages and disadvantages of lipid-emulsion administration, the current situation in Japan, and differences between lipid formulations. Here, we address issues regarding lipid-emulsion use, including: administration rate, drug mixing, administration in critically ill patients, and early postoperative use. Our findings suggest the following solutions to each issue: although a rate below 0.1 g/kg/hr is generally recommended, faster administration is possible if needed, depending on the case; administration via a piggy tube to basic infusion formulations is unproblematic; second- and third-generation fat emulsions are safe for critically ill patients, though soybean oil should be used with caution; and while fat emulsion administration is feasible immediately after surgery, due to endogenous energy mobilization, it is preferable to initiate administration from the third to fourth postoperative day.
Conclusion
The provisional conclusions of this study are as follows: the introduction of medium-chain triglyceride formulations and fish oil (second- and third-generation lipid emulsions), which are not yet available in Japan, is urgently needed; and individualized administration is essential due to substantial interindividual variability in lipid emulsion usage.
- 4,288 View
- 30 Download

- Postoperative gut dysbiosis and its clinical implications, with an emphasis on probiotic strategies in gastric cancer patients undergoing gastrectomy: a narrative review
- Cheong Ah Oh
- Ann Clin Nutr Metab 2025;17(2):114-124. Published online August 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0023
-
 Abstract
Abstract
 PDF
PDF - Purpose
This review explores alterations in gut microbiota following gastrointestinal surgery, with a focus on gastrectomy for gastric cancer, and evaluates the therapeutic potential of probiotics in restoring microbial balance and reducing postoperative complications, including infections, inflammation, immune dysfunction, and cancer recurrence.
Current concept
Gastrointestinal surgery disrupts gut microbial homeostasis via surgical stress, oxygen exposure, altered bile flow, and perioperative antibiotic use. Gastrectomy, in particular, induces marked changes in the microbiota, including increased oral-origin and aerotolerant bacteria, decreased short-chain fatty acid–producing species, and elevated bile acid-transforming organisms. These alterations contribute to complications such as small intestinal bacterial overgrowth, surgical site infections, postoperative ileus, nutrient malabsorption, and potentially a higher risk of colorectal cancer. Probiotics—especially strains of Lactobacillus, Bifidobacterium, and Clostridium—have demonstrated beneficial effects by modulating the gut ecosystem, enhancing epithelial barrier integrity, and regulating immune and metabolic pathways. Randomized clinical trials support using probiotics in improving gastrointestinal recovery, reducing systemic inflammation, restoring microbial diversity, and shortening hospital stays after gastrectomy. Multi-strain probiotic formulations, particularly when administered perioperatively, show the greatest promise. However, safety concerns remain, especially for immunocompromised or critically ill patients, underscoring the need for rigorous clinical oversight and adherence to regulatory standards such as the European Food Safety Authority’s Qualified Presumption of Safety guidelines.
Conclusion
Postoperative dysbiosis is a modifiable factor in adverse surgical outcomes. Probiotic supplementation offers promising therapeutic potential in patients undergoing gastrectomy, though optimal strains, dosing, and timing remain to be determined. Tailored, evidence-based strategies may ultimately enhance both recovery and long-term outcomes after gastric cancer surgery.
- 8,561 View
- 55 Download

Original Articles
- Evaluation of the modified Nutrition Risk in Critically Ill score in Korean critically ill patients with COVID-19: a retrospective cohort study
- Won Ho Han, Jong-Mog Lee, Jae Hoon Lee, Hyun Mi Lee, Ji-Yeon Kim, Mok Young Jang, Sung-Sik Han
- Ann Clin Nutr Metab 2025;17(2):125-131. Published online August 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0009
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Purpose
We evaluated the efficacy of the modified Nutrition Risk in Critically Ill (mNUTRIC) score for malnutrition screening and its association with mortality in intensive care unit (ICU) patients with COVID-19.
Methods
The nutritional status of 129 COVID-19 ICU patients admitted between February 2021 and May 2022 was assessed using American Society for Parenteral and Enteral Nutrition/Academy of Nutrition and Dietetics (ASPEN/AND) criteria. The sensitivity, specificity, and clinical correlations of the mNUTRIC score were analyzed.
Results
Of the 129 patients, 35 (27.1%) met the ASPEN/AND malnutrition criteria. Multivariable analysis identified the mNUTRIC score, underlying malignancy, and mechanical ventilation as significant factors associated with malnutrition. The mNUTRIC score had a sensitivity of 77.1% and specificity of 63.8% (area under the curve [AUC], 0.71; 95% confidence interval [CI], 0.62–0.79) for diagnosing malnutrition, improving to 88.6% and 80.9%, respectively, after adjusting for malignancy and ventilation (AUC, 0.89; 95% CI, 0.82–0.95). Patients with a low mNUTRIC score had a mortality rate of 2.9% and a median ICU stay of 7.7 days (range, 0–84.2 days), whereas those with a high score (≥5) had a mortality rate of 13.1% and a median ICU stay of 10.2 days (range, 1.4–88.5 days) (P=0.046 and P=0.011, respectively).
Conclusion
The mNUTRIC score is an effective screening tool for malnutrition in ICU patients with COVID-19, especially those with malignancy or requiring mechanical ventilation, and is strongly associated with mortality and length of ICU stay.
- 2,779 View
- 30 Download

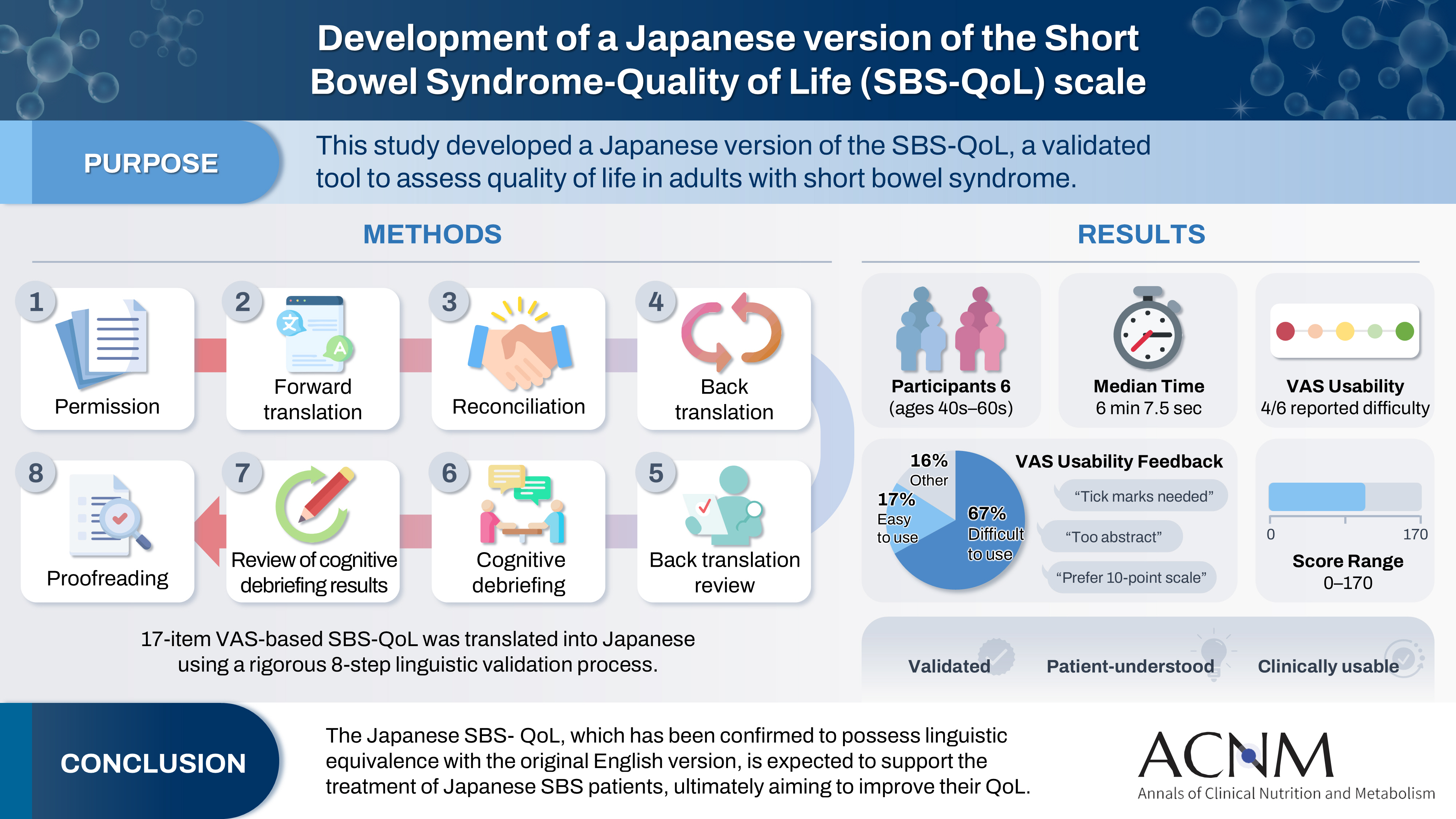
- Development of a Japanese version of the Short Bowel Syndrome-Quality of Life (SBS-QoL) scale
- Yuko Tazuke, Mayu Suzuki, Sae Kikuchi, Kaori Ishiguro, Hiroomi Okuyama
- Ann Clin Nutr Metab 2025;17(2):132-138. Published online August 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0016
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 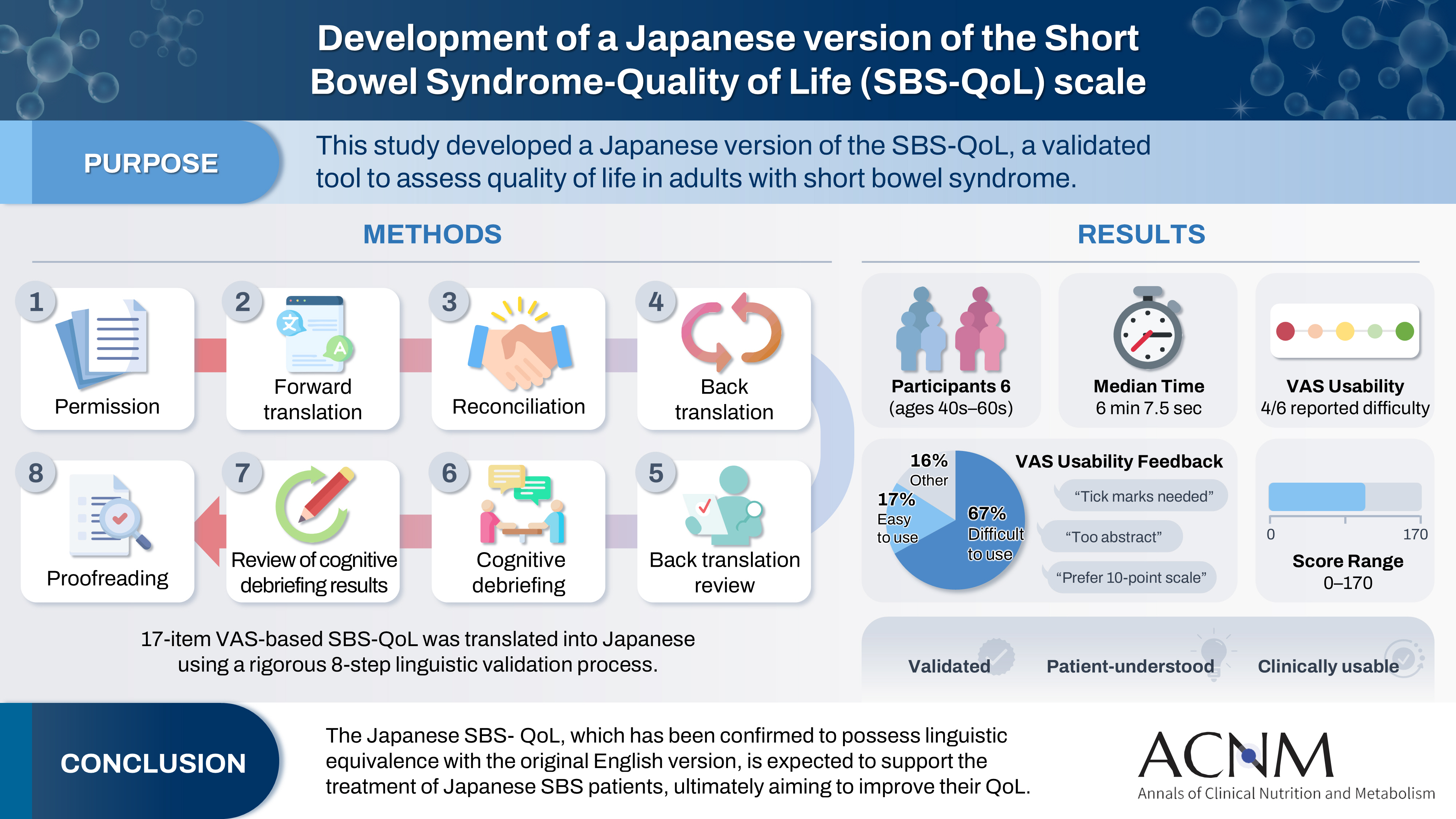
- Purpose
The Short Bowel Syndrome‐Quality of Life (SBS‐QoL) scale is a reliable and sensitive instrument developed to measure and evaluate the quality of life (QoL) in adult patients with short bowel syndrome (SBS). In Japan, increasing attention has been given to the assessment of QoL in patients with SBS; however, no Japanese‐language SBS‐specific scale is currently available. This study aimed to develop a Japanese version of the SBS‐QoL based on the original English version.
Methods
A provisional Japanese version was created in accordance with the guidelines of the International Society for Pharmacoeconomics and Outcomes Research (ISPOR) Task Force, utilizing a process of forward translation, adjustment, and back translation.
Results
Cognitive debriefing using the provisional Japanese version was conducted with six Japanese patients with SBS. Based on these results, the Japanese wording was evaluated and revised, leading to the creation of the final Japanese version.
Conclusion
The Japanese SBS‐QoL, which has been confirmed to possess linguistic equivalence with the original English version, is expected to support the treatment of Japanese SBS patients, ultimately aiming to improve their QoL.
- 1,642 View
- 19 Download

- Insulinotropic action of L-carnitine and branched-chain amino acids following energy intake in healthy, young Japanese women: a non-randomized controlled trial
- Yoichi Sakurai, Hideyuki Namba, Satoshi Odo
- Ann Clin Nutr Metab 2025;17(2):139-148. Published online August 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0011
-
 Abstract
Abstract
 PDF
PDF - Purpose
The present study uses healthy human volunteers to examine the insulinotropic action of L-carnitine and branched-chain amino acids (BCAAs) after energy intake.
Methods
A total of 39 young, healthy human volunteers were assigned to receive oral doses of either L-carnitine alone (L group, n=10) or L-carnitine combined with a single or long-term continuous dose of BCAAs. Controls (C group, n=16) received none of these. L-carnitine was administered orally at 1,000 mg/d for 14 days, and BCAA was administered orally either once just before exercise (L+SB group, n=6), or every day for 14 days (L+CB group, n=7) until 2 days before the experiment. After overnight fasting, 200 kcal of glucose and oral nutritional supplement were administered to prevent hypoglycemia. Blood glucose, free-fatty acid, and serum insulin levels were measured to examine the insulinotropic action before and after exercise.
Results
Blood glucose and serum insulin levels in the L group were significantly lower than those in the C group. While the serum insulin levels were higher after energy administration than those in the fasting state in all groups, these were significantly higher in the L+SB group and in the L+CB group compared with those in the L group. The insulinotropic action after energy intake remained even after the repeated administration of BCAA discontinued 2 days before the experi¬ment and even after serum BCAA levels remained the same.
Conclusion
While the insulinotropic action appeared after a single dose of BCAA, it was also potentiated by long-term repeated oral administration of BCAA.
- 940 View
- 13 Download

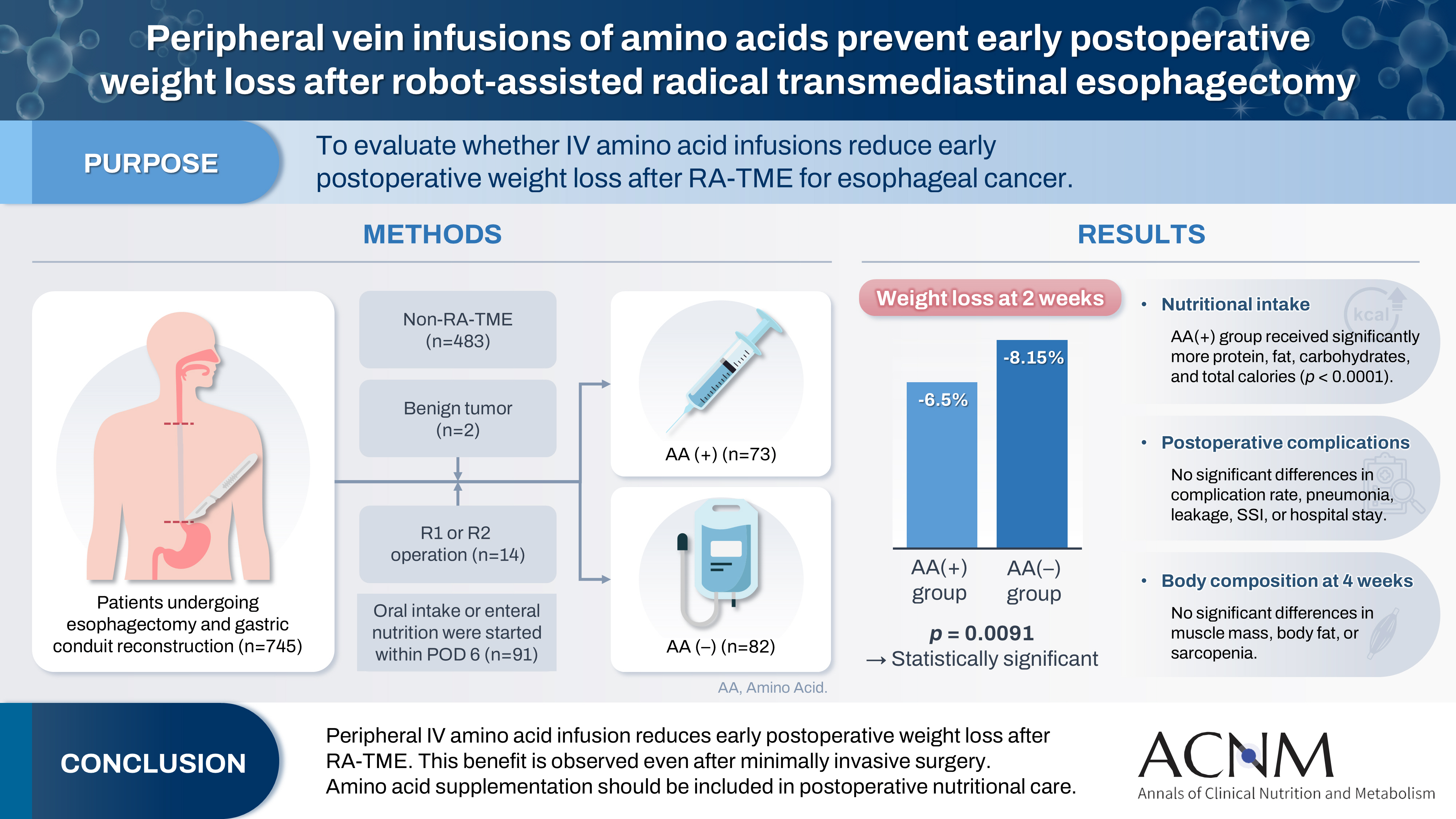
- Peripheral vein infusions of amino acids prevent early postoperative weight loss after robot-assisted radical transmediastinal esophagectomy: a retrospective study in Japan
- Tomonori Narita, Kazuhiko Fukatsu, Satoshi Murakoshi, Reo Inoue, Kenichi Kono, Midori Noguchi, Nana Matsumoto, Shoh Yajima, Koichi Yagi, Yoshifumi Baba
- Ann Clin Nutr Metab 2025;17(2):149-155. Published online August 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0012
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material 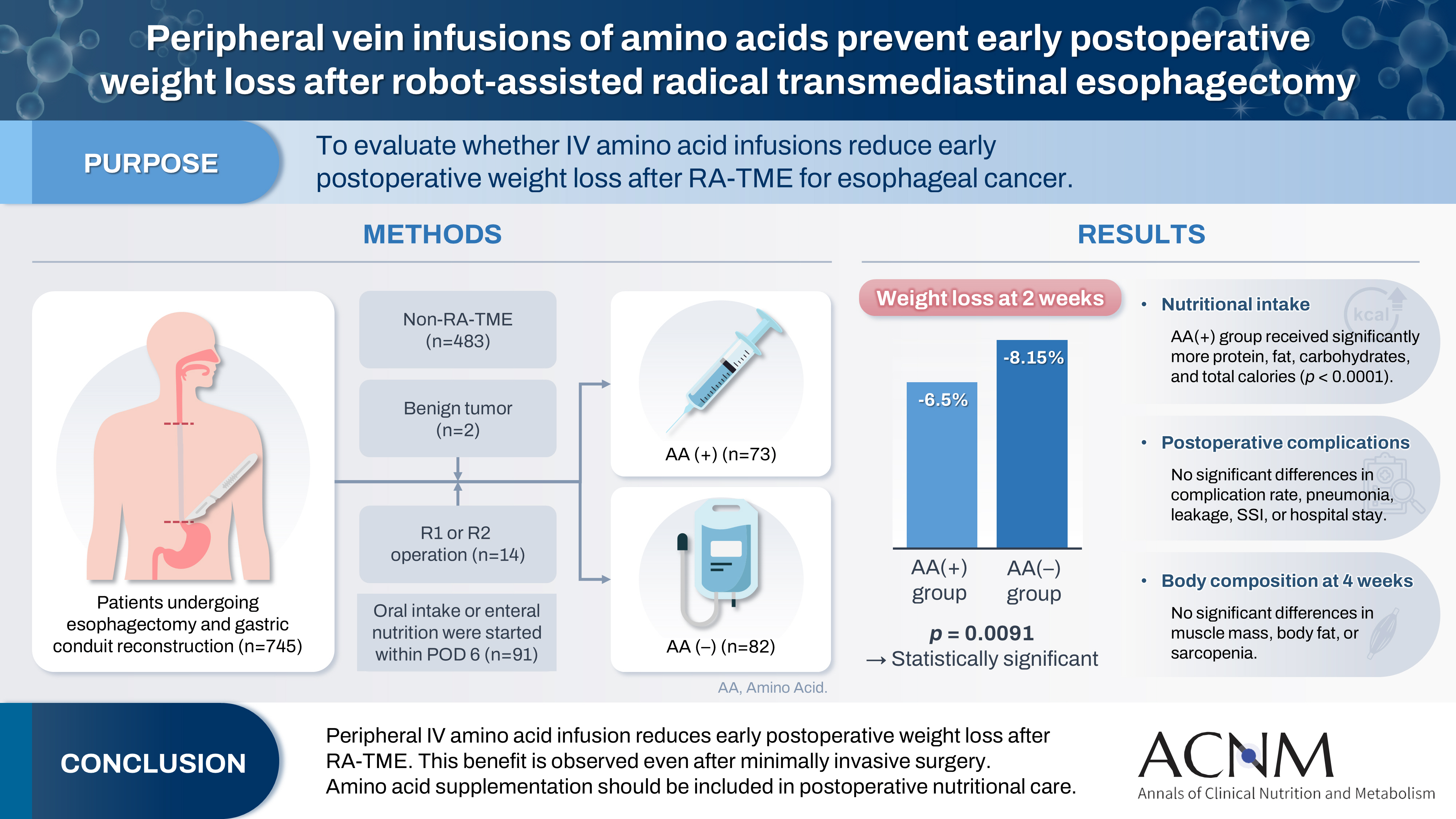
- Purpose
Postoperative body weight loss (PBWL) is linked to poor long-term outcomes following esophagectomy for esophageal cancer, making perioperative nutrition critically important. Although minimally invasive procedures such as robot-assisted radical transmediastinal esophagectomy (RA-TME) have become more prevalent, less attention has been paid to perioperative nutritional management. This study evaluates the impact of intravenous (IV) amino acid infusions on PBWL in patients undergoing RA-TME.
Methods
We retrospectively analyzed 155 patients who underwent RA-TME for esophageal or esophagogastric junction cancer at our hospital between 2011 and 2022. Patients were divided into two groups: AA(+) (n=73, received IV amino acids between postoperative days 1–6) and AA(–) (n=82, did not receive IV amino acids). Oral or enteral nutrition was withheld until postoperative day 6. We compared nutrient intake, postoperative outcomes, and nutritional status between groups.
Results
Patient backgrounds, surgical outcomes, and complication rates were similar in both groups. However, the AA(+) group received significantly greater energy and nutrient intake. PBWL at 2 weeks post-surgery was significantly lower in the AA(+) group than in the AA(–) group (6.50% vs. 8.15%, P=0.0091).
Conclusion
IV amino acid infusion may help mitigate early PBWL after RA-TME.
- 1,195 View
- 17 Download

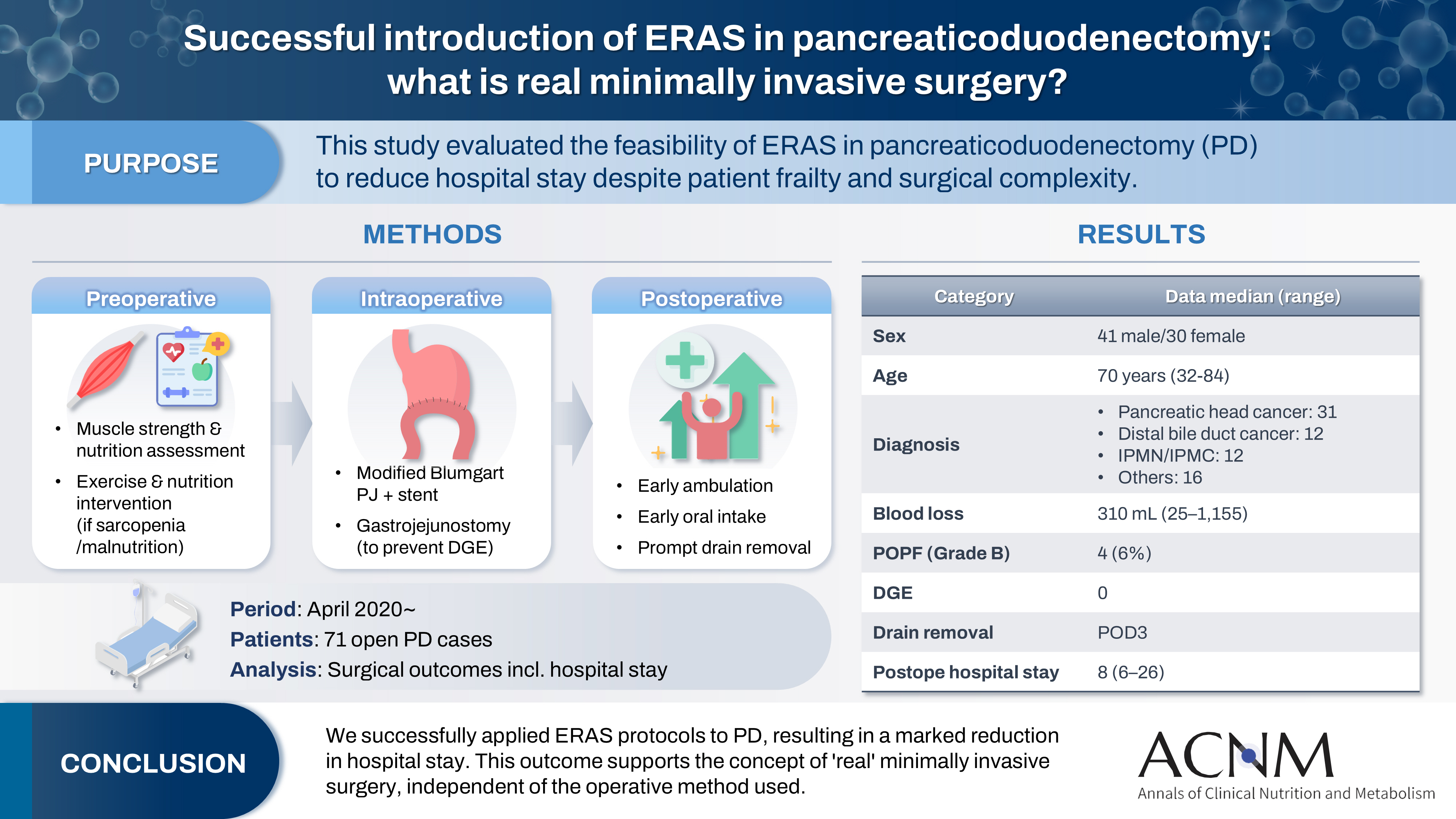
- Successful introduction of ERAS in pancreaticoduodenectomy: what is real minimally invasive surgery?
- Toshimi Kaido, Yosuke Miyachi, Koichiro Mitsuoka, Mariko Sambommatsu
- Ann Clin Nutr Metab 2025;17(2):156-161. Published online August 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0014
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 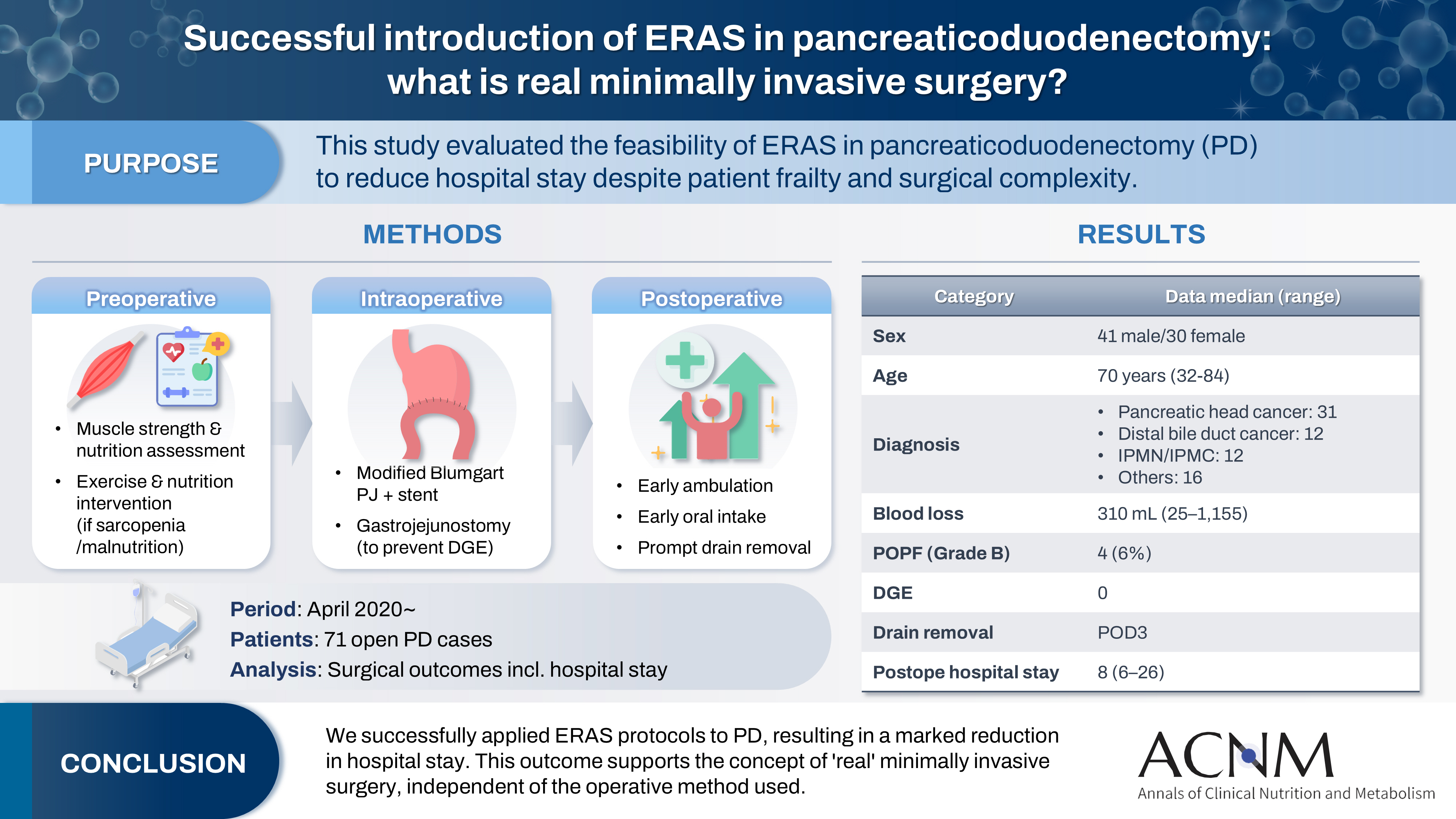
- Purpose
The introduction of Enhanced Recovery After Surgery (ERAS) protocols for pancreaticoduodenectomy (PD) has been considered challenging due to factors such as preexisting malnutrition, sarcopenia, the complexity of the surgery, and the high incidence of postoperative complications, including postoperative pancreatic fistula (POPF) and delayed gastric emptying (DGE). This study aimed to determine whether ERAS could be implemented in PD to achieve shorter postoperative hospital stays.
Methods
Our novel approach consists of three components. Preoperatively, we routinely assess patients' muscle strength and nutritional status and initiate exercise and nutritional interventions for those identified with sarcopenia or malnutrition. Intraoperatively, we perform pancreaticojejunostomy using a modified Blumgart’s technique with our stent placement policy and utilize new gastrojejunostomy methods to prevent DGE. Principles of postoperative management are early ambulation, early oral intake, and early drain removal. Since April 2020, we have employed this strategy and retrospectively evaluated its effectiveness. We enrolled 71 consecutive patients who underwent open PD with curative intent. Various surgical outcomes, including postoperative hospital stay, were analyzed.
Results
There were 41 men and 30 women, with a median age of 70 years. Preoperative diagnoses included pancreatic head cancer in 31, distal bile duct cancer in 12, and others. Median intraoperative blood loss was 310 mL. Grade B POPF occurred in four patients (6%). No cases of DGE were observed. The median postoperative hospital stay was 8 days (range, 6–26 days).
Conclusion
We successfully implemented ERAS protocols in PD and achieved a significantly reduced postoperative hospital stay. We propose that this approach is “real minimally invasive surgery," regardless of the surgical technique used.
- 3,777 View
- 18 Download


 E-submission
E-submission KSPEN
KSPEN KSSMN
KSSMN ASSMN
ASSMN JSSMN
JSSMN


 First
First Prev
Prev


